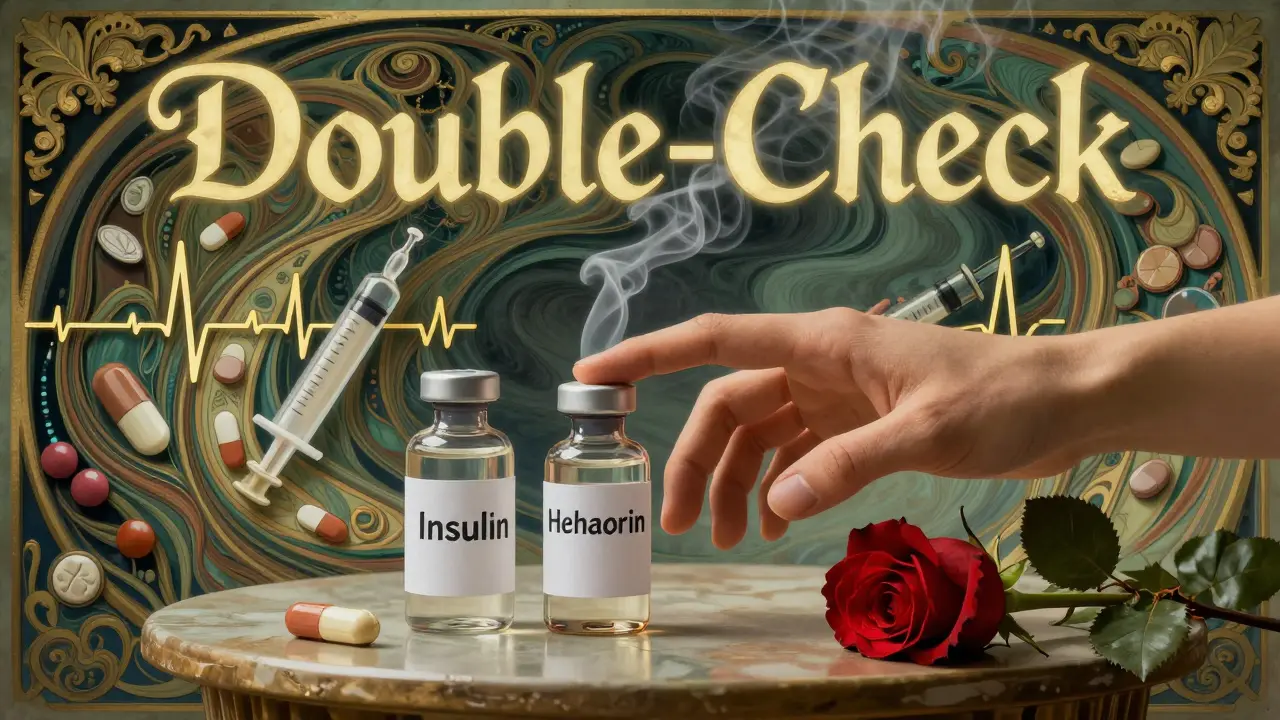
Look-Alike, Sound-Alike Medication Names That Cause Errors: Real Risks and How to Stop Them

Dec, 29 2025
Imagine this: a nurse grabs a vial from the shelf, reads the label, and administers what she thinks is levothyroxine. But it’s Synthroid. Same thing, right? Wrong. In some hospitals, those two names are treated as different drugs - and mixing them up has led to serious overdoses. This isn’t a rare mistake. It’s happening every day in clinics, pharmacies, and hospitals - and it’s mostly because of look-alike, sound-alike (LASA) drug names.
What Exactly Are LASA Medications?
LASA stands for look-alike, sound-alike. These are medications that either look similar on the label, sound alike when spoken, or come in nearly identical packaging. The problem isn’t that the drugs are the same - it’s that they’re dangerously different. For example:- Hydromorphone (a strong opioid painkiller) vs. hydrocodone (a weaker painkiller often paired with acetaminophen)
- Doxorubicin (a chemotherapy drug) vs. daunorubicin (also chemo, but used for different cancers)
- Clonazepam (an anti-seizure and anxiety med) vs. clonidine (a blood pressure drug)
Why Do These Errors Keep Happening?
You’d think after decades of warnings, hospitals would have fixed this. But they haven’t. Here’s why:- Verbal orders are risky. When a doctor says “synthroid” over the phone, the pharmacist hears “levothyroxine.” Both are thyroid meds. Both are common. Both are stored near each other. One mistake = wrong dose, wrong patient outcome.
- High workload = mental shortcuts. During busy shifts, especially at night or during shift changes, staff rush. They rely on memory, not double-checks. A 2022 study found that 78% of doctors had a near-miss with LASA drugs in just one year.
- Similar packaging. Many drugs come in identical blue or white bottles with the same font size and layout. Even if the name is printed clearly, the eye skips to the shape, color, or logo - not the text.
- New drugs keep getting approved with confusing names. The FDA denied 34 new drug names in 2022 because they were too similar to existing ones. But that’s only a fraction of what’s out there. Some companies still push names that are phonetically close - and regulators are slow to catch them.
The Real Cost: Deaths, Not Just Mistakes
These aren’t just near-misses. People die from LASA errors. The FDA’s MAUDE database shows at least 128 deaths linked to drug name confusion between 2018 and 2022. Most involved high-alert drugs:- Insulin - confused with heparin, leading to fatal hypoglycemia
- Neuromuscular blockers like vecuronium - mistaken for versed (a sedative), causing paralysis during surgery
- Anticoagulants like warfarin - confused with other blood thinners, leading to uncontrolled bleeding

What’s Being Done - And Why It’s Not Enough
There are solutions. But most are half-measures. Tall Man Lettering - where part of the drug name is capitalized to highlight differences - is used on over 200 drug pairs in the U.S. For example:- HYDROmorphone vs. hYDROcodone
- cisPLATIN vs. caraPLATIN
What Actually Works: Proven Strategies
If you’re a pharmacist, nurse, or doctor, here’s what you can do - right now - to reduce risk:- Always spell out drug names. Never say “synthroid.” Say “S-Y-N-T-H-R-O-I-D.” Spell it like you’re talking to someone who’s hard of hearing.
- Use the “read-back” rule. When receiving a verbal order, repeat it back word-for-word. “You want 5 mg of HYDROmorphone?”
- Check the vial, not just the label. Look at the pill color, shape, imprint. If it doesn’t match what you expect, stop. Ask.
- Know your high-alert drugs. Insulin, opioids, heparin, chemo - these are the big ones. Treat them like live grenades. Double-check every time.
- Push for Tall Man Lettering in your EHR. If your system doesn’t use it, ask why. If they say “it’s not standard,” show them the FDA list.
The Future: AI, Regulation, and Better Design
The good news? Change is coming - slowly. The FDA is now testing AI-powered voice recognition systems that can catch LASA errors during verbal orders. Early results from Johns Hopkins show 89% accuracy in spotting risky pairs like “morphine” vs. “hydromorphone.” The WHO and the International Pharmaceutical Federation are pushing for global standards: no more drug names that sound like existing ones. By 2030, they want all new medications to pass strict naming tests before approval. And in 2024, ISMP added 12 new dangerous pairs to its High-Alert LASA List - including melphalan and meloxicam. One’s chemotherapy. The other’s a painkiller. Mix them up? You’re risking organ failure.You Can’t Trust the System - So Don’t
The truth is, no system is foolproof. Not the EHR. Not the label. Not the pharmacist’s memory. Even with all the rules, errors still happen. The only thing that keeps patients safe is you - the person holding the medication, the one who pauses for a second to ask, “Is this right?” If you’re a patient: ask your pharmacist to spell out the drug name. If you’re a provider: slow down. Say it out loud. Check the vial. Double-check the dose. Because in the end, LASA errors aren’t about bad software or lazy staff. They’re about human attention - and how easily it breaks under pressure. Don’t assume it won’t happen to you. It already has - to someone nearby. And it will again - unless you’re the one who stops it.What are the most dangerous look-alike, sound-alike drug pairs?
The most dangerous pairs involve high-alert medications. Examples include: HYDROmorphone vs. hYDROcodone (opioid overdose risk), doxorubicin vs. daunorubicin (chemotherapy mix-ups), vecuronium vs. versed (paralysis during sedation), and insulin vs. heparin (fatal hypoglycemia or bleeding). These combinations have caused deaths even in well-run hospitals.
Does Tall Man Lettering really prevent errors?
Tall Man Lettering helps - but only if staff are trained to notice it. Studies show it reduces errors by about 10-15% when used correctly. But in many places, it’s ignored because people don’t know what it’s for. It’s not a fix - it’s a reminder. The real solution is combining it with verbal confirmation and electronic alerts.
Why do new drugs keep getting confusing names?
Drug companies often choose names that sound professional or marketable - not safe. The FDA reviews names, but the process is slow and under-resourced. In 2022, the FDA blocked 34 new names for being too similar to existing ones. But hundreds of confusing names are still on the market. Regulatory pressure is increasing, but change moves slowly.
How often do LASA errors happen?
About one in four medication errors in the U.S. is due to drug name confusion, according to Medscape and the Anesthesia Patient Safety Foundation. In hospitals, LASA-related errors account for up to 65% of all medication name mix-ups. Many go unreported because they’re caught before harm occurs - but the near-misses are far more common than the actual injuries.
What should patients do to protect themselves?
Always ask your pharmacist to spell out the drug name. Check the pill against the description on the label - color, shape, imprint. If you’re given a new medication, compare it to the last one you took. If it looks different, ask why. Don’t assume it’s the same drug just because the name sounds familiar.
Are electronic health records helping reduce LASA errors?
Yes - but only in places that use them well. Systems like Epic and Cerner now have built-in LASA alerts that flag similar names during prescribing. One study showed a 28.7% drop in errors after implementation. But many small clinics still use paper or outdated software. The gap in safety between big hospitals and small ones is wide - and dangerous.
