Skin Parasites: Their Growing Impact on the Medical Community

Oct, 5 2025
Skin Parasite Diagnosis Checker
Enter patient information and click "Analyze Potential Parasite" to get diagnostic insights.
- Scabies: Intense nocturnal itching with burrows in web spaces
- Cutaneous Larva Migrans: Serpiginous, erythematous tracks on feet or thighs
- Strongyloidiasis: Urticarial rash or larva currens in immunosuppressed patients
- Myiasis: Furuncular lesions with moving larvae
- Demodicosis: Rosacea-like papules or blepharitis
When doctors talk about skin parasites organisms that live on or lay eggs beneath the human epidermis, causing a range of dermatological and systemic problems, they’re not just describing an odd annoyance - they’re highlighting a public‑health challenge that reshapes diagnostics, treatment protocols, and research funding.
What counts as a skin‑dwelling parasite?
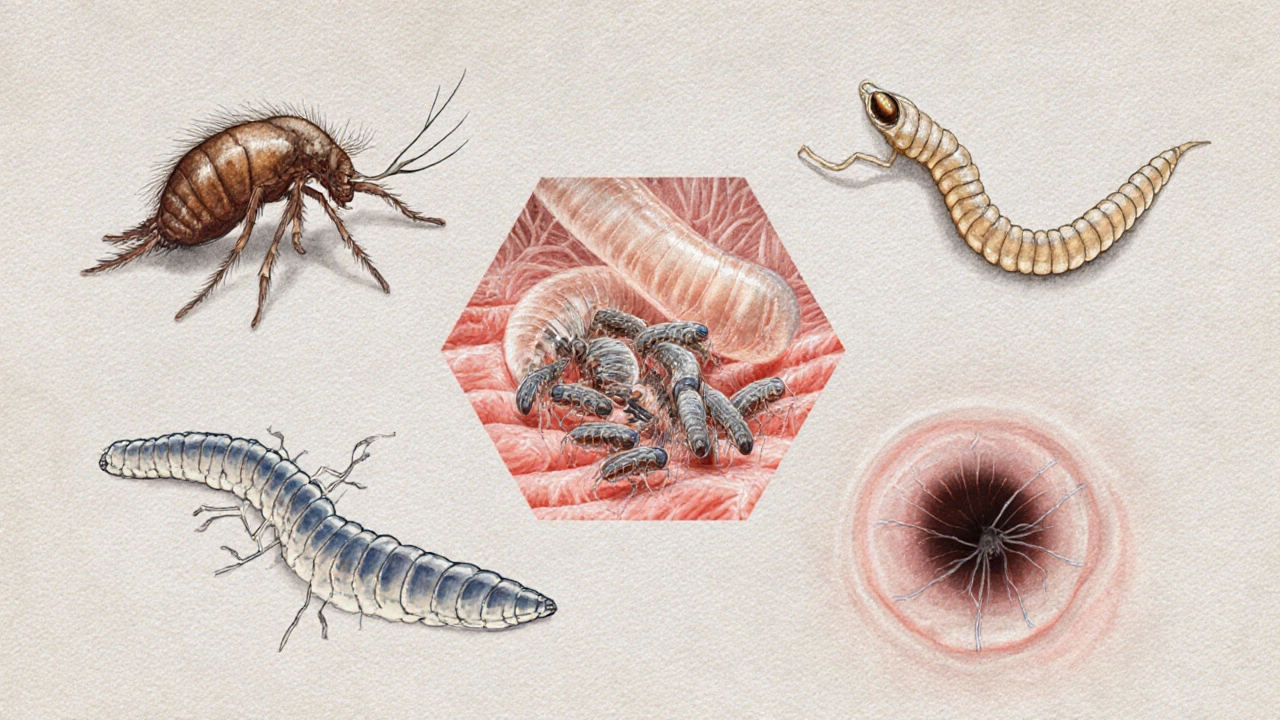
Skin parasites include arthropods, nematodes, and even some protozoa that either burrow into the epidermis or migrate just beneath it. The most common culprits are:
- Sarcoptes scabiei the mite that causes scabies, burrowing into the skin to lay eggs
- Ancylostoma braziliense a hookworm species responsible for cutaneous larva migrans, moving through the dermis
- Strongyloides stercoralis a threadworm that can autoinfect and cause chronic skin rashes
- Myiasis‑causing flies larvae that feed on necrotic tissue or invade healthy skin
- Demodex folliculorum microscopic mites that inhabit hair follicles, linked to rosacea and blepharitis
Clinical impact: From misdiagnosis to severe complications
Why do these tiny organisms matter to clinicians? Because the skin is a gateway - an infection that starts there can quickly become systemic. Consider these real‑world scenarios:
- Scabies outbreaks in nursing homes - Elderly patients often present with atypical itching that mimics eczema. Missed diagnosis leads to rapid spread, increased morbidity, and costly isolation measures.
- Cutaneous larva migrans in travelers - Beachgoers from temperate zones return with serpiginous tracks. Without recognition, they may receive unnecessary antibiotics instead of a single dose of ivermectin.
- Strongyloidiasis in immunosuppressed patients - A patient on corticosteroids develops a hyperinfection syndrome, presenting with diffuse rash, pneumonia, and sepsis. Early identification saves lives.
- Myiasis in diabetic foot ulcers - Larvae accelerate tissue destruction, complicating wound healing and raising amputation risk.
- Demodex overgrowth in rosacea - Infamous for being dismissed as “bad skin,” yet targeted therapy (e.g., ivermectin cream) dramatically improves symptoms.
These examples illustrate how skin parasites drive diagnostic uncertainty, prolong clinic visits, and inflate healthcare costs.
How the medical community is responding
Faced with rising case numbers-especially in tropical regions and among travelers-health systems are adapting in four key ways:
- Guideline updates: The American Academy of Dermatology (AAD) and WHO have revised treatment algorithms to prioritize oral ivermectin over topical permethrin for resistant scabies.
- Training emphasis: Medical schools now include dedicated modules on parasitic skin diseases, using high‑resolution dermoscopy images to differentiate mite burrows from fungal hyphae.
- Surveillance programs: Public‑health agencies in Australia, the US, and Europe track outbreak clusters via electronic health records, allowing rapid response teams to deploy topical scabicides in shelters.
- Research funding: Grants are flowing into vaccine development for hookworm and novel anti‑helmintic compounds that could also work on cutaneous stages.
Emerging trends that clinicians must watch
Three forces are reshaping the landscape of skin‑dwelling parasites:
- Climate change: Warmer temperatures expand the geographic range of hookworm larvae, making cutaneous larva migrans a concern even in previously temperate zones.
- Global travel: More than 1.4billion international trips were recorded in 2024; each journey carries a risk of exposure to endemic parasites, prompting dermatologists to ask detailed travel histories.
- Urban wildlife: Growing populations of stray cats and dogs in cities elevate the local burden of fleas and hookworms, linking veterinary and human health in a One‑Health framework.
Staying ahead means incorporating these trends into patient counseling and public‑health policy.
Practical checklist for clinicians
- Ask about recent travel, beach exposure, and animal contact during skin examinations.
- Inspect for characteristic lesions: burrows (scabies), serpiginous tracks (larva migrans), papulopustular eruptions (myiasis).
- Use dermoscopy or skin scraping for definitive identification when possible.
- Prescribe evidence‑based treatments: oral ivermectin (200µg/kg, single dose or repeat) for scabies and larva migrans; topical permethrin 5% for uncomplicated scabies; albendazole for strongyloidiasis in immunocompromised hosts.
- Educate patients on hygiene: wash bedding at 60°C, avoid walking barefoot on sandy beaches, and use protective footwear in endemic areas.

Comparison of common skin parasites
| Parasite | Causative organism | Transmission route | Typical skin manifestation | First‑line treatment |
|---|---|---|---|---|
| Scabies | Sarcoptes scabiei (mite) | Skin‑to‑skin contact | Intense nocturnal itching, burrows in webs of fingers | Oral ivermectin 200µg/kg ×1‑2 doses |
| Cutaneous larva migrans | Ancylostoma braziliense (hookworm larvae) | Skin contact with contaminated sand or soil | Serpiginous, erythematous tracks | Ivermectin 200µg/kg single dose |
| Strongyloidiasis | Strongyloides stercoralis (nematode) | Larvae penetrate skin, autoinfection possible | Urticarial rash, larva currens | Ivermectin 200µg/kg daily for 2days |
| Myiasis | Fly larvae (e.g., Cochliomyia hominivorax) | Eggs deposited on wound or moist skin | Furuncular lesions, sometimes moving larvae | Manual removal + antibiotics if secondary infection |
| Demodicosis | Demodex folliculorum (mite) | Endogenous, overgrowth in follicles | Rosacea‑like papules, blepharitis | Ivermectin 1% cream BID for 4‑6weeks |
Future directions: What the medical community hopes to achieve
Looking ahead, researchers aim to close three gaps:
- Rapid point‑of‑care diagnostics: Lateral‑flow tests detecting mite DNA in skin scrapings could cut diagnosis time from days to minutes.
- Resistance monitoring: Rising ivermectin resistance in scabies has prompted genomic surveillance programs similar to those used for malaria.
- Integrated One‑Health strategies: Joint human‑veterinary campaigns targeting stray animal deworming may reduce community exposure to hookworm larvae.
When these initiatives succeed, clinicians will spend less time chasing elusive bugs and more time delivering definitive care.
Frequently Asked Questions
How can I tell if my rash is caused by a skin parasite?
Look for characteristic patterns: burrows in the web spaces (scabies), winding red tracks on the foot or thigh (cutaneous larva migrans), or moving ‘boils’ that may indicate myiasis. A detailed travel and exposure history helps narrow it down.
Is ivermectin safe for children?
Ivermectin is approved for children over 15kg for scabies and over 1year of age for certain helminth infections. Doses are weight‑based, and side‑effects are usually mild (headache, nausea).
Can skin parasites cause systemic illness?
Yes. Strongyloides can lead to hyperinfection syndrome with lung and gut involvement, especially in immunosuppressed patients. Poorly treated myiasis can trigger sepsis, and severe scabies can cause secondary bacterial infections.
What preventive steps should travelers take?
Wear closed shoes on beaches, avoid sitting directly on sand, use insect repellents, and wash any skin exposed to soil with soap and water as soon as possible. For high‑risk trips, a single dose of ivermectin before travel can be discussed with a clinician.
Why are outbreaks of scabies increasing in developed countries?
Factors include crowded housing, aging populations in care facilities, and migration from endemic regions. Additionally, delayed diagnosis due to atypical presentations in the elderly fuels spread.
