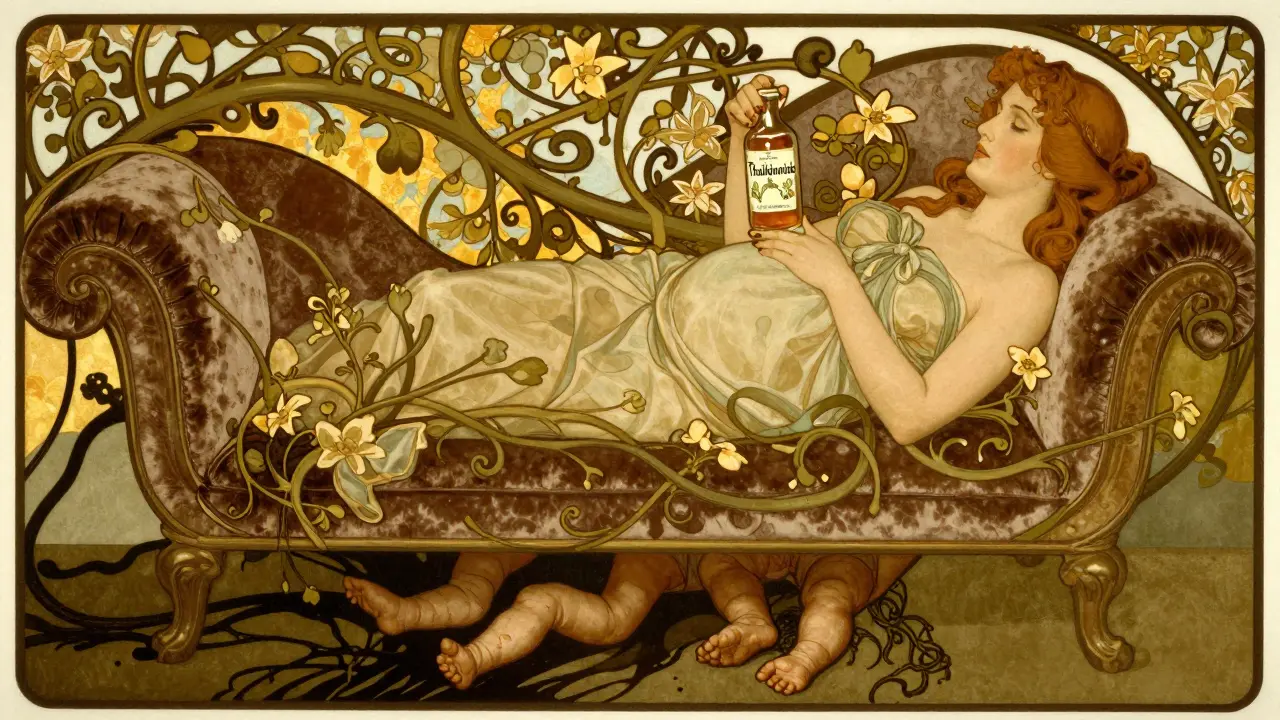
Thalidomide and Teratogenic Medications: History, Impact, and Modern Safety Lessons
Jan, 3 2026
Thalidomide is one of the most infamous drugs in medical history-not because it failed to work, but because it worked too well in the wrong way. In the late 1950s, it was sold as a safe, over-the-counter sedative and morning sickness remedy for pregnant women. By 1961, thousands of babies were born with missing or stunted limbs, deafness, blindness, and internal organ damage. The tragedy didn’t happen because doctors were careless. It happened because no one tested whether the drug could harm a developing fetus.
How a ‘Safe’ Drug Became a Disaster
Thalidomide was developed in West Germany in 1954 by Chemie Grünenthal. It was marketed as a gentle, non-addictive alternative to barbiturates. Ads claimed it was safe enough for pregnant women. By 1958, it was available in 46 countries. In Australia, Canada, the UK, and across Europe, it was prescribed freely to ease nausea and help sleep. At the time, there were no rules requiring drug makers to prove their products were safe for unborn babies. Testing for fetal harm? Not done.
The first known case was a baby born with phocomelia-limbs that looked like flippers-on Christmas Day, 1956, in Germany. No one connected the dots. Birth defects were common, and doctors assumed they were genetic or random. But by 1960, doctors in Germany and Australia started noticing a pattern. Babies with the same rare deformities were being born in clusters, and their mothers had all taken thalidomide during early pregnancy.
The Two Doctors Who Stopped the Tragedy
In Australia, Dr. William McBride, a pediatrician at the Women’s Hospital in Sydney, noticed an unusual spike in limb deformities. He wrote a letter to The Lancet in June 1961, directly linking thalidomide to the birth defects. Around the same time, in Germany, Dr. Widukind Lenz, a medical geneticist, had been tracking the same pattern in his clinic. He called Grünenthal on November 15, 1961, and told them: ‘Your drug is causing these defects.’
Germany pulled thalidomide off the market on November 27. The UK followed on December 2. But in the United States, the disaster was narrowly avoided. A young FDA reviewer named Frances Oldham Kelsey refused to approve the drug. She asked for more data on safety in pregnancy. The company, Richardson-Merrell, pressured her for months. She held firm. Her skepticism saved thousands of American babies.
What Exactly Did Thalidomide Do to Babies?
Thalidomide doesn’t cause random birth defects. It targets a very specific window: between 34 and 49 days after the last menstrual period. That’s when limbs, ears, eyes, and internal organs are forming. A single dose during this time could be enough to cause irreversible damage.
Children born with thalidomide exposure had:
- Phocomelia: arms or legs that were severely shortened or absent
- Missing thumbs or fingers
- Facial paralysis or cleft palate
- Deafness or blindness
- Heart defects, kidney malformations, or missing organs like the gallbladder
- Neurological damage that showed up later-some children developed seizures or intellectual disabilities
About 40% of affected infants died before their first birthday. Survivors faced lifelong disabilities. Many were abandoned by families or institutionalized. The UK government’s 1964 report confirmed that thalidomide could damage nearly every organ system. There was no safe dose. No safe time. Just a brutal, silent window of destruction.

Why Didn’t Animal Testing Catch It?
Drug companies tested thalidomide on rats and mice. Nothing happened. No birth defects. So they assumed it was safe. But here’s the key: thalidomide only causes birth defects in humans, rabbits, and a few primates. Mice and rats don’t metabolize it the same way. The tests were useless. And when McBride asked the University of Sydney to test it on pregnant rabbits, his request was denied. The professor said it was unnecessary.
This wasn’t negligence. It was ignorance. Scientists didn’t know that species differ in how drugs affect fetal development. The tragedy forced a global rethink: if you’re testing a drug for pregnant women, you must test it on species that respond like humans.
The Regulatory Revolution That Followed
Before thalidomide, drug approval was a formality. Companies submitted basic data. If it looked harmless, it got approved. After 1962, everything changed.
In the U.S., Congress passed the Kefauver-Harris Amendments. For the first time, drug makers had to prove:
- That their drug was effective, not just safe
- That it was tested for teratogenicity-harm to unborn babies
- That side effects were clearly disclosed
Other countries followed. The UK created the Committee on the Safety of Medicines. The World Health Organization began requiring fetal toxicity studies. Suddenly, every new drug had to pass a battery of pregnancy tests. The thalidomide tragedy didn’t just change one drug’s fate-it rewrote the entire system of drug safety.
Thalidomide’s Dark Comeback
By the 1980s, thalidomide was considered a relic of medical horror. Then, in 1964, an Israeli doctor named Jacob Sheskin gave it to a leprosy patient with painful skin sores-and the sores vanished. No one knew why. But it worked.
Decades later, researchers discovered the secret: thalidomide blocks blood vessel growth. Tumors need new blood vessels to survive. Thalidomide starves them. It also calms the immune system. That’s why it helped leprosy patients (erythema nodosum leprosum) and later, people with multiple myeloma, a deadly bone marrow cancer.
In 1998, the FDA approved it for leprosy. In 2006, it was approved for myeloma. Clinical trials showed it improved survival: 86% of patients were alive after three years with thalidomide, compared to 75% without. But it came with a cost. Up to 60% of patients developed nerve damage-numbness, tingling, pain in hands and feet. Many had to stop taking it.

How Is It Used Today-And Why Is It So Strictly Controlled?
Thalidomide is still sold today. But it’s not in pharmacies. It’s not prescribed casually. It’s only available through a strict program called STEPS (System for Thalidomide Education and Prescribing Safety).
Here’s what it takes to get it now:
- Women of childbearing age must use two forms of birth control
- They must take monthly pregnancy tests
- They must sign forms acknowledging the risks
- Men taking it must use condoms-thalidomide can be in semen
- Doctors must be certified to prescribe it
- Pharmacies must be registered to dispense it
Why? Because even today, thalidomide remains one of the most potent human teratogens known. A single pill, taken during early pregnancy, can still cause devastating birth defects. The science behind it is now clear: thalidomide binds to a protein called cereblon, which is essential for limb development. It breaks down the signals that tell a fetus how to grow arms and legs. One molecule. One mistake. One life changed forever.
What We Learned-And What We Still Forget
Thalidomide taught us that drugs aren’t just for adults. They can cross the placenta. They can alter fetal DNA. They can destroy a life before it begins. We now test every new drug for fetal risk. We warn women. We track outcomes. We have systems.
But the lessons are still being ignored. In 2020, the WHO reported that over 7% of birth defects globally are linked to medications taken during pregnancy. Many are still untested. Many are still prescribed without warning. In some countries, pregnant women still take painkillers, antibiotics, or antidepressants without knowing the risks.
Thalidomide wasn’t just a mistake. It was a warning. And warnings only matter if we listen.
The Legacy: From Tragedy to Teaching Tool
Today, thalidomide is taught in every medical school, pharmacy program, and public health course. The Science Museum in London has a permanent exhibit on it. Survivors have become advocates. Their stories are part of the curriculum.
It’s not just about history. It’s about responsibility. Every time a drug is approved, someone must ask: ‘What if a pregnant woman takes this?’ That question saved lives after thalidomide. We can’t stop asking it now.
Was thalidomide ever approved in the United States?
No, thalidomide was never approved for general sale in the United States. FDA reviewer Frances Oldham Kelsey refused to approve it in the late 1950s and early 1960s because the safety data, especially for pregnant women, was incomplete. Her decision prevented a widespread outbreak of birth defects in the U.S., even as thousands of children were affected in other countries.
Can thalidomide be used safely during pregnancy today?
No. Thalidomide is strictly contraindicated during pregnancy. Even a single dose during the first trimester can cause severe birth defects. Today, it is only prescribed under the STEPS program, which requires mandatory contraception, pregnancy testing, and patient education. No exceptions are made.
Are there other drugs like thalidomide that can cause birth defects?
Yes. Other known teratogens include isotretinoin (Accutane) for acne, valproic acid for epilepsy, and certain anticoagulants like warfarin. Each has a specific window of risk during pregnancy. Today, all new drugs undergo fetal toxicity testing, and warnings are required if a drug is known to harm unborn babies.
Why did it take so long to realize thalidomide caused birth defects?
The critical window for damage was narrow-between weeks 4 and 8 of pregnancy-and birth defects were often blamed on genetics or random chance. Also, the drug was taken for weeks or months, so doctors didn’t connect it to a single exposure. Plus, animal tests didn’t show harm, so the medical community assumed it was safe. It took careful observation by two doctors to spot the pattern.
Is thalidomide still used today, and if so, for what?
Yes, thalidomide is still used today, but only under strict controls. It is approved for treating erythema nodosum leprosum (a complication of leprosy) and multiple myeloma, a type of blood cancer. It works by suppressing inflammation and blocking tumor blood vessel growth. Annual global sales are around $300 million, almost entirely for cancer treatment.
How did the thalidomide tragedy change how drugs are tested?
Before thalidomide, drug companies didn’t need to prove effectiveness or test for fetal harm. Afterward, the U.S. passed the Kefauver-Harris Amendments in 1962, requiring proof of both safety and efficacy. All new drugs must now undergo rigorous testing for teratogenicity, especially if they’re intended for use in women of childbearing age. Similar rules were adopted worldwide.
