AKI on CKD: How to Avoid Contrast and Nephrotoxic Medications
Feb, 16 2026
What Happens When AKI Strikes on Top of CKD?
Imagine your kidneys are already working at 40% capacity because of chronic kidney disease (CKD). Then, you get an infection, take a new painkiller, or need a CT scan with contrast dye. Suddenly, your kidney function drops another 30% in just a few days. This isn’t just a bad day-it’s acute kidney injury (AKI) on top of CKD, and it’s one of the most dangerous scenarios in nephrology. The risk of death jumps. The chance of needing dialysis rises. And the damage? It might not come back.
Every year, tens of thousands of people with CKD suffer AKI after being exposed to common medications or imaging dyes. Many of these cases are preventable. The key isn’t complex science-it’s knowing what to avoid and when.
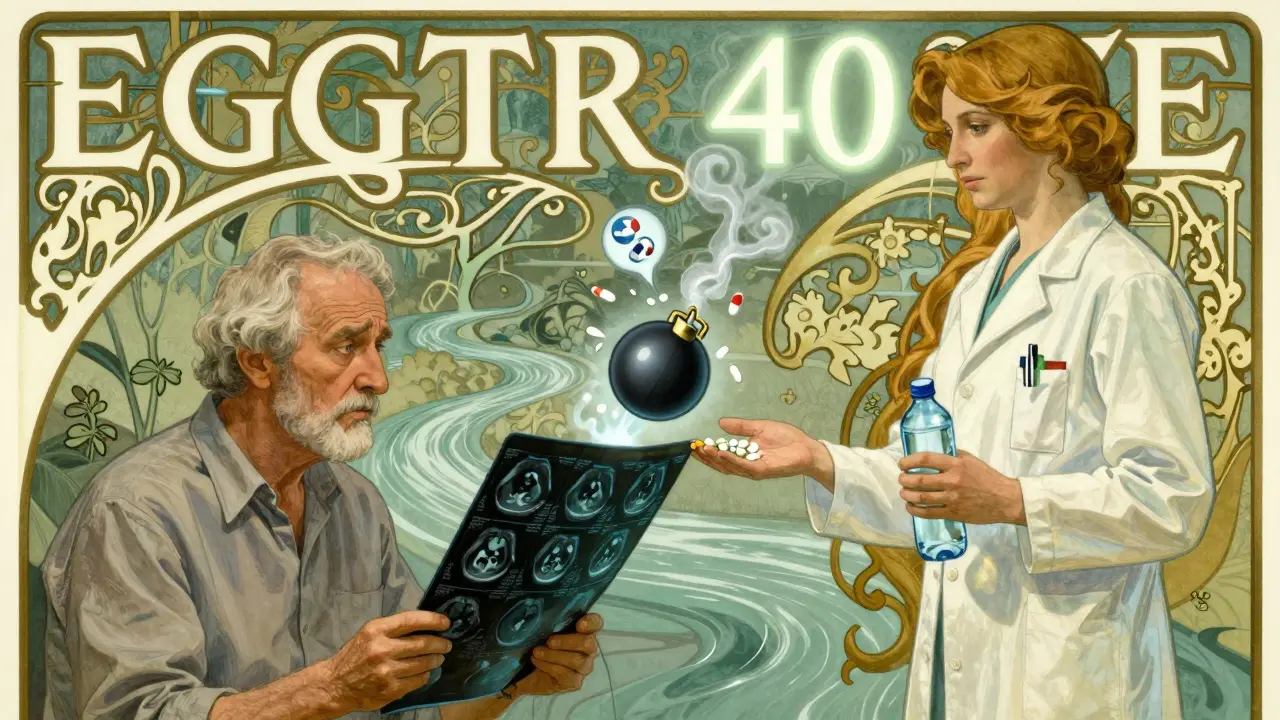
Why Contrast Dye Is a Silent Threat
Iodinated contrast dye is used in CT scans, angiograms, and other imaging tests to make blood vessels and organs show up clearly. It’s safe for most people. But for someone with CKD? It’s a landmine.
According to the KDIGO 2012 guidelines, patients with CKD stages 3 to 5 (eGFR below 60 mL/min/1.73m²) have a 12% to 50% chance of developing contrast-induced AKI (CI-AKI). That’s not a small number-it’s a high-risk gamble. People with diabetes and CKD? Their risk hits 20-50%. Add heart failure or dehydration, and the numbers climb even higher.
The problem isn’t the dye itself. It’s how the kidneys react. Contrast dye reduces blood flow to the inner part of the kidney, where filtering happens. In a healthy kidney, this is temporary. In a damaged one? It can trigger cell death, inflammation, and lasting injury.
Here’s what the guidelines say: avoid contrast when possible. If you absolutely need it, use the smallest dose-usually no more than 100 mL. And never skip hydration. Drinking water or getting IV fluids at 1.0-1.5 mL/kg/hour for 6-12 hours before and after the scan can cut your risk by 30-40%.
Some doctors still use sodium bicarbonate or N-acetylcysteine (NAC) to protect the kidneys. But recent studies show these don’t work better than plain saline. Stick to isotonic fluids. No magic pills. No fancy protocols. Just fluids, low dose, and time.
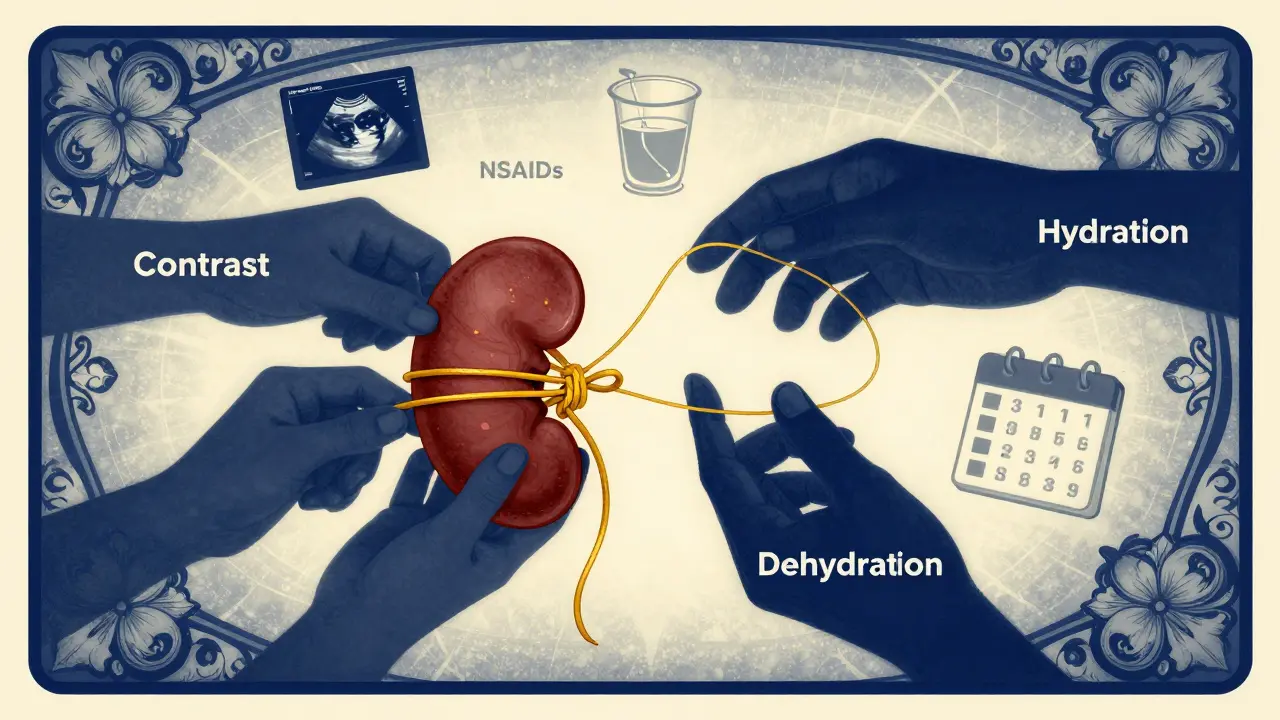
The Medications That Hurt More Than They Help
Contrast isn’t the only danger. Many common drugs are quietly damaging kidneys in people with CKD.
NSAIDs-like ibuprofen, naproxen, and celecoxib-are the biggest offenders. They block protective chemicals in the kidney that help maintain blood flow. In someone with CKD, this can cause sudden, severe AKI. Studies show NSAID use in CKD patients increases AKI risk by 2.5 times. A 2020 study in the American Journal of Kidney Diseases found that patients who got clear counseling about avoiding NSAIDs had 25% fewer hospitalizations for kidney injury.
ACE inhibitors and ARBs (like lisinopril or losartan) are usually good for CKD. They protect the kidneys long-term. But during an acute illness or dehydration, they can cause a dangerous drop in kidney filtration. If you’re sick, dehydrated, or on diuretics, your doctor should temporarily hold these medications. A 15-25% rise in creatinine after starting or restarting them isn’t a mistake-it’s a warning sign.
Aminoglycosides (gentamicin, tobramycin) and vancomycin are antibiotics used for serious infections. But they’re toxic to kidney cells. Vancomycin toxicity spikes when blood levels go above 15 mcg/mL. That’s why doctors check levels and adjust doses. In CKD patients, even standard doses can be too much.
Amphotericin B, used for fungal infections, is one of the most nephrotoxic drugs out there-up to 80% of patients on it develop some kidney damage. Alternatives like echinocandins are safer, but often more expensive. When cost isn’t an issue, choose the gentler option.
And don’t forget diuretics. Many patients with CKD are on them for swelling. But if you’re in AKI, they don’t help. In fact, KDIGO says they shouldn’t be used to prevent or treat AKI unless you’re clearly fluid-overloaded. They just make things worse.
What to Do When You’re Already in AKI
If you’ve been diagnosed with AKI on CKD, the clock is ticking. The goal isn’t to fix the injury-it’s to stop it from getting worse.
First: stop all nephrotoxic drugs. That includes NSAIDs, contrast, antibiotics like vancomycin, and even some herbal supplements. A 2021 study from Duke University found that discontinuing these agents prevented 30-50% of AKI cases from progressing to severe stages.
Second: reassess all medications. Many drugs are cleared by the kidneys. If your kidney function dropped from eGFR 45 to 25 in a week, your dose of metformin, digoxin, or certain antibiotics needs to change. Don’t rely on your old CKD dose. Use your current kidney function. Pharmacists can help with this. Studies show pharmacist-led reviews cut AKI rates in hospitalized CKD patients by 22%.
Third: monitor closely. In stable CKD, creatinine is checked every 3-6 months. In AKI on CKD, check it every 24-48 hours. Urine output matters too. If you’re making less than 0.5 mL/kg/hour for more than 6 hours, that’s a red flag.
Fourth: don’t rush into dialysis. The 2022 AKIKI 2 trial showed that early dialysis doesn’t improve survival in severe AKI on CKD. Wait for clear signs of toxicity-high potassium, acidosis, fluid overload-before starting. Aggressive dialysis doesn’t save kidneys. It just replaces function.
What’s New in Kidney Protection
The KDIGO guidelines from 2012 are still the gold standard. But science is moving fast.
One big shift: the idea of Acute Kidney Disease (AKD). If your kidney function is low for more than 7 days but less than 3 months, it’s not just AKI anymore. It’s AKD. This means you need different follow-up. After an AKI episode, your doctor should check your eGFR and urine albumin-to-creatinine ratio (uACR) again in 3 months. You might be sliding into permanent damage.
Another change: new biomarkers. Tests for TIMP-2 and IGFBP7 can predict AKI within 12 hours-long before creatinine rises. These aren’t routine yet, but they’re coming. In ICUs, they’re already being used to catch injury before it’s too late.
And hydration? Still the best tool. No evidence supports sodium bicarbonate over normal saline. No benefit from dopamine or fenoldopam. Just fluids. Simple. Effective.
How to Protect Yourself
If you have CKD, here’s your action list:
- Always tell every doctor you see that you have CKD-even your dentist.
- Never take NSAIDs without asking your doctor first. Use acetaminophen instead for pain.
- If you need imaging, ask: “Is contrast absolutely necessary? Can we use ultrasound or MRI instead?”
- Stay hydrated. Especially when you’re sick, hot, or on diuretics.
- Keep a list of all your meds and review it with your pharmacist every 3 months.
- Know your eGFR and uACR numbers. Ask for them at every visit.
- If you’re hospitalized, ask if a nephrologist has been consulted. Studies show 20% lower death rates when they are.
One patient I spoke to-68, CKD stage 4, diabetic-had two AKI episodes in two years. Both happened after she took ibuprofen for back pain and got a CT scan without hydration. The second time, she needed dialysis for 3 weeks. She didn’t know her kidneys were that fragile. She does now.
Who’s at Highest Risk?
Not everyone with CKD is equally at risk. These groups need the most caution:
- Diabetes + CKD (risk: 20-50% for CI-AKI)
- Heart failure + CKD (risk: 15-35%)
- Dehydrated or volume-depleted patients
- Those on multiple nephrotoxic drugs
- Older adults (over 75) with reduced muscle mass (creatinine can be misleading)
Even if your eGFR is 40, if you’re on three nephrotoxic drugs and haven’t had a drink in two days? You’re in danger. It’s not just the number-it’s the combo.
Final Thought: Prevention Is Simple, But Not Easy
There’s no miracle drug for AKI on CKD. No new pill. No breakthrough surgery. The best treatment is avoidance. Avoid contrast. Avoid NSAIDs. Avoid dehydration. Avoid unnecessary drugs.
It sounds basic. But in hospitals, 30-50% of CKD patients aren’t even flagged as high-risk before they get a nephrotoxic drug. Electronic alerts help-but 40% of doctors override them because they think they know better. They don’t.
The real solution? Communication. Between you and your doctor. Between your pharmacist and your nurse. Between your primary care team and the radiologist.
When you have CKD, your kidneys are already hanging by a thread. Every unnecessary drug, every contrast scan, every missed fluid is a tug on that thread. Don’t let it break.
Frequently Asked Questions
Can I still get a CT scan if I have CKD?
Yes-but only if absolutely necessary. Always ask if an alternative like ultrasound or MRI is possible. If contrast is needed, use the lowest dose (usually ≤100 mL) and get IV hydration before and after. Never skip hydration. Tell the radiology team about your CKD so they can plan accordingly.
Are all painkillers dangerous for CKD patients?
No. NSAIDs like ibuprofen, naproxen, and aspirin are risky and should be avoided. Acetaminophen (Tylenol) is generally safe at normal doses (up to 3,000 mg/day). But even acetaminophen can be harmful if you have severe liver disease or drink alcohol regularly. Always check with your doctor before starting any new painkiller.
Should I stop my ACE inhibitor or ARB during an illness?
Sometimes. If you’re dehydrated, vomiting, have diarrhea, or are taking diuretics, your kidney’s blood flow drops. ACE inhibitors and ARBs can make this worse, causing a sudden rise in creatinine. Talk to your doctor. They may advise you to pause the medication for a few days until you’re back to normal. Don’t stop it on your own.
How do I know if I’m dehydrated?
Signs include dark yellow urine, dry mouth, dizziness when standing, and less frequent urination. In CKD, you might not feel thirsty even when you’re dehydrated. Drink water regularly-even if you don’t feel thirsty. Aim for at least 1.5-2 liters a day unless your doctor says otherwise. Avoid alcohol and caffeine, which can worsen dehydration.
Is N-acetylcysteine (NAC) effective for preventing AKI?
Some studies show a small benefit, but others don’t. The KDIGO guidelines say evidence is conflicting. Hydration with normal saline is more reliable and has stronger proof. NAC isn’t harmful, but it shouldn’t replace fluids. Don’t rely on it as your main protection.
Can AKI on CKD lead to permanent kidney damage?
Yes. About 30% of AKI episodes in CKD patients lead to permanent kidney function loss. Up to 15% progress to end-stage kidney disease within five years. That’s why prevention is so critical. Every avoidable AKI episode increases your long-term risk.
What should I do if I develop AKI?
Stop all nonessential medications, especially NSAIDs and nephrotoxic drugs. Stay hydrated. Get your creatinine and urine output checked daily. Ask for a nephrology consult if you’re in the hospital. Don’t assume you’ll bounce back. Monitor closely and follow up with your doctor in 3 months to check for signs of chronic kidney disease.
Do children with CKD have the same risks?
Children with CKD have lower rates of contrast-induced AKI (5-15%) than adults, but when it happens, it can be more severe. They’re also more sensitive to dehydration. Always ensure proper hydration before imaging. Dosing of medications must be adjusted by weight and kidney function. Pediatric nephrologists should be involved in care planning.
