Cognitive Behavioral Therapy: The Proven Psychological Treatment for Anxiety, Depression, and More
Nov, 24 2025
When you're stuck in a loop of negative thoughts-constantly worrying, blaming yourself, or expecting the worst-there's a reason it feels impossible to just "snap out of it." Your mind isn't broken. It's learned a pattern. And the good news? You can unlearn it. That's where cognitive behavioral therapy comes in. It's not magic. It's not vague talk about childhood trauma. It's a practical, step-by-step method backed by over 2,000 clinical studies. More than any other therapy, CBT has been tested, measured, and proven to work.
How CBT Actually Works
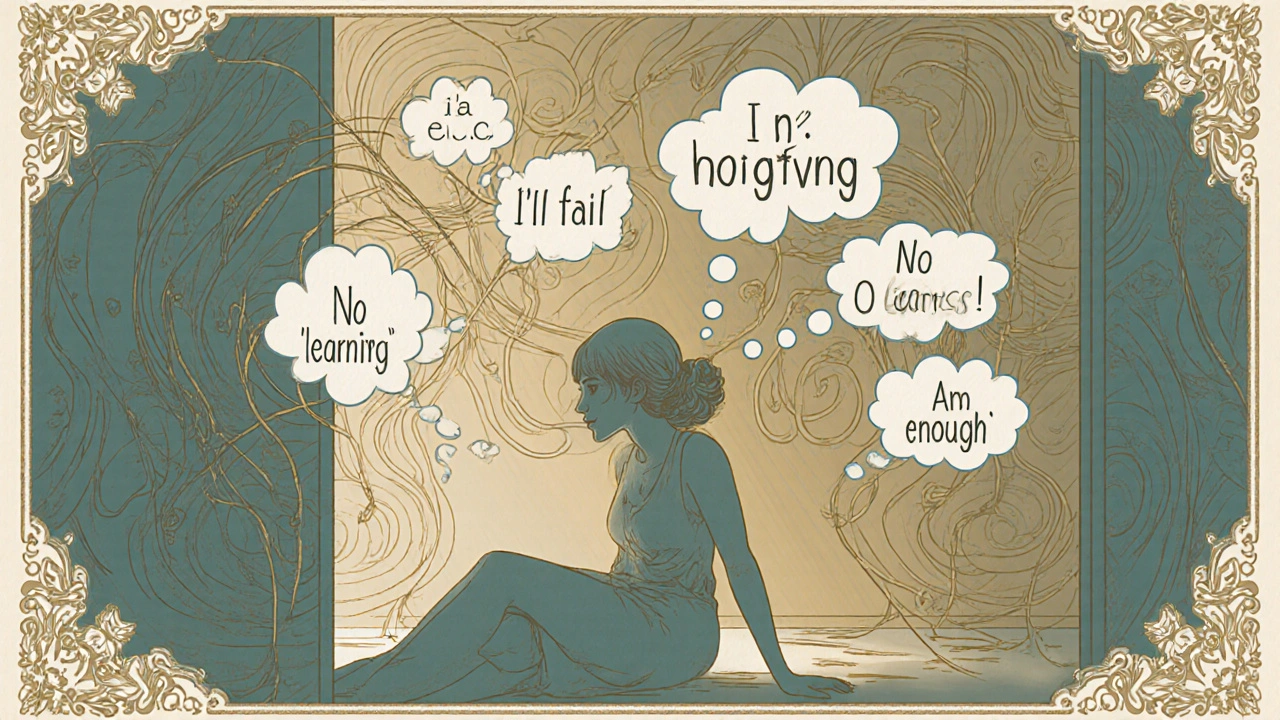
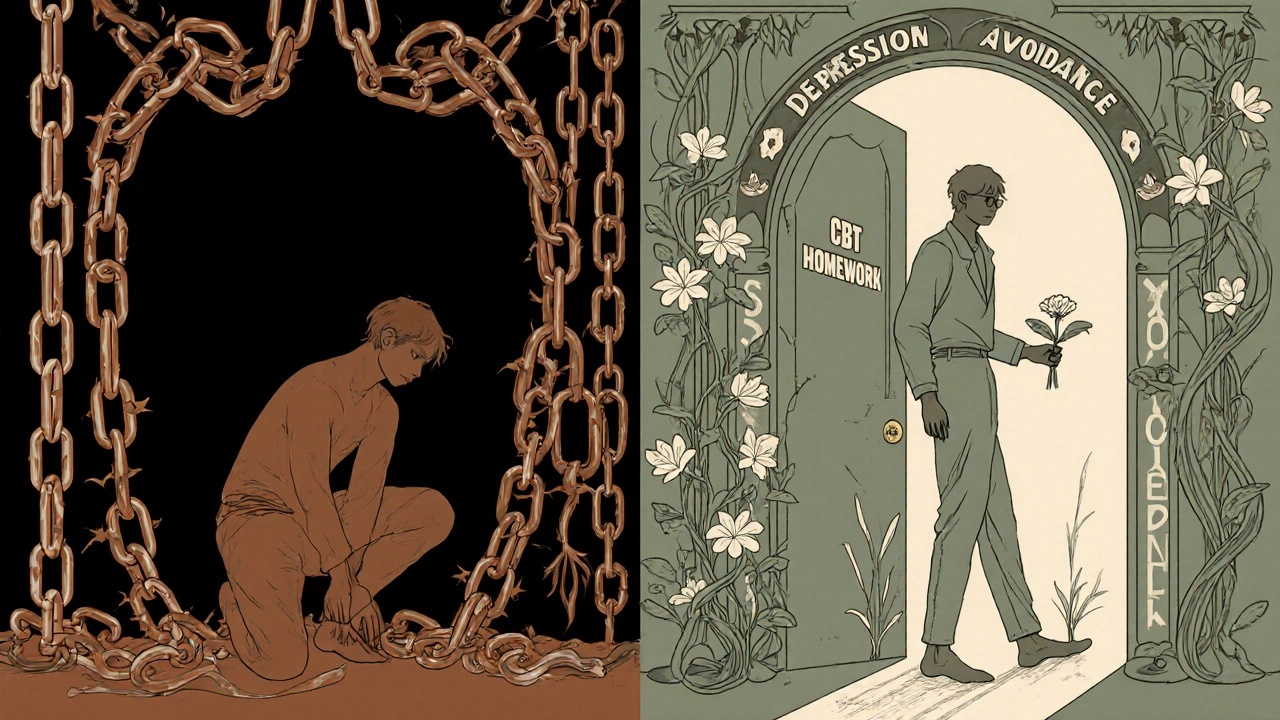
CBT doesn’t focus on why you feel bad. It asks: What are you thinking right now, and what are you doing about it? The core idea is simple: your thoughts, feelings, and actions are connected. If you think, "I’m going to fail," you feel anxious. That anxiety makes you avoid the situation. Avoidance gives you short-term relief, but it reinforces the fear. CBT breaks that cycle.
It combines two parts: cognitive (how you think) and behavioral (what you do). A therapist helps you spot distorted thinking-like assuming the worst, overgeneralizing, or mind-reading-and tests those thoughts against reality. Then, you take small, real-world actions to prove your fears wrong. For example, someone afraid of social situations might start by saying hello to a neighbor, then progress to joining a small group. Each step is a experiment, not a guess.
This isn’t theoretical. In 2018, a major analysis in JAMA Psychiatry found that 60-80% of people with anxiety disorders saw major improvement after 12-16 sessions of CBT. That’s not "maybe helped." That’s measurable, repeatable change.
What Conditions Does CBT Help With?
CBT isn’t a one-size-fits-all. It’s a toolkit. Different techniques are used for different problems:
- Anxiety disorders: Exposure therapy gradually faces fears (like public speaking or crowded places) in a controlled way. Studies show it reduces panic attacks by up to 70%.
- Depression: The "cognitive triad"-negative views of yourself, the world, and the future-is targeted with thought records. Patients track thoughts like "I’m worthless" and find evidence that contradicts them.
- PTSD: Trauma-focused CBT helps process memories without getting overwhelmed. Veterans and survivors report fewer flashbacks and nightmares after 12-15 sessions.
- OCD: Exposure and Response Prevention (ERP) is the gold standard. Instead of washing hands 20 times, you delay it-then delay it longer. A 2022 study showed 85% of patients with OCD had symptom reduction after ERP.
- Substance use: CBT teaches coping skills for cravings. People learn to recognize triggers (stress, certain people, places) and replace drinking or using with healthier habits. Success rates are 40-60% at six months, far higher than 12-step programs alone.
- Insomnia: CBT-I (Cognitive Behavioral Therapy for Insomnia) is recommended before sleeping pills. It fixes the cycle of worrying about sleep, which keeps you awake.
The National Institute for Health and Care Excellence (NICE) in the UK lists CBT as a first-line treatment for 12 conditions-from panic disorder to eating disorders. In Australia, the NHS-style public health system offers CBT through mental health programs. It’s not experimental. It’s standard care.
How Long Does It Take? What’s the Commitment?
Most CBT programs last between 8 and 20 weeks. Sessions are usually 45-60 minutes, once a week. That’s it. No years of weekly visits. No lying on a couch talking about your mom.
But here’s the catch: CBT requires work outside the room. You’ll get homework. Not because therapists are mean, but because change happens in real life. You might be asked to:
- Write down three negative thoughts each day and challenge them
- Track your mood and what triggered it
- Try a feared situation for five minutes and note what actually happened
These tasks take 15-20 minutes a day. That’s less time than scrolling through social media. But they’re the reason CBT works. One person on HealthUnlocked shared that after 10 weeks of tracking thoughts and doing exposure exercises, their social anxiety panic attacks dropped from 15 a week to just 2. That’s not luck. That’s practice.
Completion rates are high-74% in NHS England’s 2023 survey. But if you skip homework, results drop. That’s why therapists use motivational interviewing to help you stay on track. It’s not about being perfect. It’s about showing up, even when it’s hard.

How Does CBT Compare to Medication?
Many people wonder: Should I take pills or do therapy?
The answer isn’t either/or. It’s both-or one first. For mild to moderate depression, CBT alone works as well as antidepressants. The NIMH’s STAR*D trial found that after 12 months, people who did CBT had a 52% remission rate versus 47% for medication. But here’s the kicker: relapse rates were half as high with CBT (24% vs. 52%). That’s because CBT teaches skills. Pills mask symptoms.
For severe depression or bipolar disorder, medication is often needed first to stabilize mood. Then CBT helps rebuild thinking patterns. For anxiety, CBT often comes first. It’s safer, longer-lasting, and doesn’t have side effects like weight gain, drowsiness, or sexual dysfunction.
And for substance use? CBT beats medication in long-term abstinence. One study showed 55% stayed sober after six months with CBT, compared to 38% with medication alone.
Who Might Not Benefit?
CBT isn’t for everyone. It works best when you can think clearly, reflect on your thoughts, and commit to practice. It’s less effective for:
- People with severe cognitive impairment (like advanced dementia)
- Those in acute psychosis or severe mania
- Individuals with complex trauma and deep emotional dysregulation
For borderline personality disorder, Dialectical Behavior Therapy (DBT)-which evolved from CBT-works better. For young children with behavioral issues, Parent-Child Interaction Therapy (PCIT) shows stronger results. And for chronic pain, newer "third-wave" CBT approaches like Acceptance and Commitment Therapy (ACT) are more effective.
Also, if you’re not ready to face your fears or challenge your thoughts, CBT can feel frustrating. That’s normal. Good therapists check in and adjust. But if you’re looking for a therapy where you just talk and feel heard, CBT might not be the fit.
What Do People Actually Say About It?
Real people, not studies. On Psychology Today, 87% of 1,243 reviews rated CBT as "very effective" or "extremely effective" for anxiety. Reddit users in r/mentalhealth praised "thought records" and "behavioral experiments" as the most helpful tools. One user wrote: "I used to avoid phone calls. After 12 sessions, I called my boss to ask for a raise. I got it. That’s not therapy. That’s life change."
But it’s not all smooth. About 32% of negative reviews mention homework as overwhelming. And 27% say exposure exercises felt too scary at first. That’s part of the process. It’s not supposed to feel easy. It’s supposed to feel like growth.
How to Find a CBT Therapist
Not all therapists are trained in CBT. Look for:
- Certification from the Academy of Cognitive Therapy
- Training from the Beck Institute (the original CBT center)
- Use of structured manuals like the Cognitive Therapy Scale
In Australia, many public mental health services offer CBT through government-funded programs. Private practitioners usually charge $100-$180 per session. Some health insurance plans cover it. Check your policy.
There are also digital options. Woebot, an FDA-cleared CBT chatbot, has over 2 million users. But studies show in-person CBT is 22% more effective. Apps are great for support, but not replacement.
The Future of CBT
CBT isn’t stuck in the past. It’s evolving. Researchers are now using AI to analyze thought records in real time. The National Institute of Mental Health is building "precision CBT"-matching treatment to brain activity patterns. In five to seven years, you might get a CBT plan based on your heart rate, sleep data, and speech patterns.
But the core won’t change. It’s still about thoughts, behaviors, and practice. No matter how techy it gets, CBT’s power comes from one thing: you learning to be your own therapist.
Is CBT Worth It?
If you’re tired of feeling stuck, anxious, or down-and you’re ready to do the work-then yes. It’s not the easiest path. But it’s the most proven. You don’t need to understand neuroscience or philosophy. You just need to be willing to ask: "Is this thought true? What’s the evidence? What’s a better way to think?" Then take one small step.
That’s all CBT asks for. And for millions, that’s been enough to change their lives.
How long does it take to see results from CBT?
Most people start noticing changes within 4-6 weeks. For anxiety or depression, significant improvement often happens by week 8-12. The key is consistency-attending sessions and doing homework. Some conditions, like OCD or PTSD, may take longer (16-20 sessions), but progress is usually steady.
Can I do CBT on my own without a therapist?
Yes, but with limits. Self-help books, apps like Woebot, and online CBT programs can help with mild anxiety or low mood. However, for moderate to severe symptoms, working with a trained therapist leads to better outcomes. Therapists catch blind spots, adjust techniques, and provide accountability. DIY CBT works best as a supplement-not a replacement.
Is CBT just about "thinking positive"?
No. CBT doesn’t ask you to think happy thoughts. It asks you to think more accurately. If you believe "I’ll never get a job," CBT helps you examine the evidence. Maybe you’ve had rejections, but you’ve also had interviews. Maybe you haven’t applied yet. The goal isn’t to be optimistic-it’s to be realistic. That’s what reduces anxiety, not forced positivity.
Does CBT work for children and teens?
Yes, and it’s often adapted for younger clients. For kids, therapists use games, drawings, and role-play to teach skills. For teens, CBT helps with social anxiety, school stress, and depression. Success rates are slightly lower than in adults-around 63%-but still strong. Parent involvement often improves outcomes.
What if I can’t afford CBT?
Many public health systems offer free or low-cost CBT. In Australia, Medicare covers mental health sessions with a referral from your GP. Community health centers and universities often run low-fee clinics. Online resources like the National Alliance on Mental Illness (NAMI) provide free CBT workbooks. Don’t let cost stop you-options exist.
Is CBT the same as coaching or self-help?
No. Life coaches and self-help books offer general advice. CBT is a clinical treatment based on decades of research, with specific protocols for diagnosable conditions. A licensed CBT therapist follows evidence-based manuals, tracks progress with standardized tools, and adjusts treatment based on data-not intuition. It’s therapy, not motivation.
If you’ve been struggling with your thoughts or emotions for a long time, CBT offers a clear, practical path forward. It doesn’t promise quick fixes. But it does promise real change-if you’re willing to show up, write it down, and try something new.
