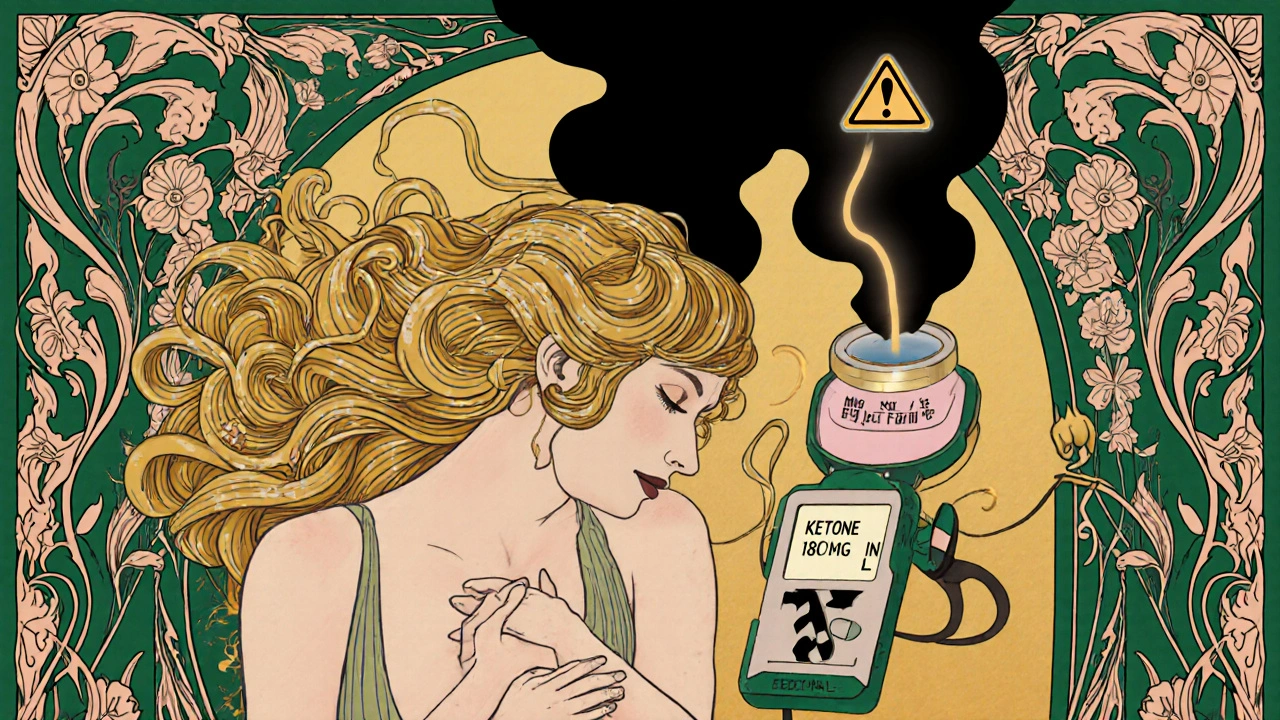
Euglycemic DKA on SGLT2 Inhibitors: How to Recognize and Treat This Hidden Emergency
Nov, 20 2025
Euglycemic DKA Risk Assessment Tool
Euglycemic DKA Risk Assessment
This tool helps you assess your risk of euglycemic diabetic ketoacidosis (DKA) while taking SGLT2 inhibitors. Remember: DKA can occur with normal blood sugar. Check your symptoms and risk factors to determine if you should seek immediate medical attention.
Your results will appear here...
Most people with diabetes know that diabetic ketoacidosis (DKA) means high blood sugar, fruity breath, and a trip to the ER. But what if your blood sugar is normal-and you’re still in DKA? This isn’t a rare glitch. It’s a real, life-threatening condition called euglycemic DKA, and it’s happening more often in people taking SGLT2 inhibitors like Farxiga, Jardiance, and Invokana.
What Is Euglycemic DKA?
Euglycemic DKA is diabetic ketoacidosis that happens without the usual spike in blood glucose. Instead of levels above 250 mg/dL, patients often have readings between 100 and 250 mg/dL-normal enough to fool even experienced providers. But their blood is still acidic, their ketones are sky-high, and their bodies are breaking down fat for fuel like they’re starving.This isn’t just a twist on classic DKA. It’s a different beast. The same triggers-illness, surgery, skipping meals, drinking alcohol-can set it off. But the drug itself plays a key role. SGLT2 inhibitors work by making your kidneys dump sugar into your urine. That lowers blood glucose. But it also tricks your body into thinking it’s low on fuel. Your pancreas responds by releasing more glucagon, less insulin. Fat breaks down. Ketones pile up. And you get acidosis-even if your glucose looks fine.
Studies show that SGLT2 inhibitors increase the risk of DKA by 7 times in people with type 2 diabetes. Even more concerning: about 20% of these cases happen in people who’ve never had DKA before. And while these drugs aren’t approved for type 1 diabetes, about 8% of type 1 patients are still taking them off-label-and their DKA rates jump to 5-12%.
Why It’s So Easy to Miss
The biggest danger? Normal blood sugar makes you feel safe. Patients often delay seeking help because they think, “My sugar’s fine, so I can’t be in DKA.” Providers do the same. A 2015 study in Diabetes Care found 13 cases where patients were misdiagnosed because their glucose levels were below 250 mg/dL. One patient was sent home with a diagnosis of “gastroenteritis.” He returned two days later in cardiac arrest.Symptoms are identical to classic DKA: nausea, vomiting, abdominal pain, extreme fatigue, rapid breathing (Kussmaul respirations), confusion. But here’s the trap: no fruity breath. No extreme thirst. No frequent urination. Just vague, flu-like symptoms that look like a stomach bug or stress.
And lab tests can be misleading. Leukocytosis (high white blood cells) is common-but it’s often from dehydration, not infection. Lactic acid can rise too, making it look like sepsis or shock. If you only check glucose and pH, you’ll miss it. You need to check ketones.
How to Diagnose It
There’s no mystery to diagnosing euglycemic DKA. It’s simple if you know to look for it:- Blood glucose below 250 mg/dL
- Arterial pH less than 7.3
- Serum bicarbonate below 18 mEq/L
- Ketones elevated (beta-hydroxybutyrate > 3 mmol/L)
Don’t rely on urine dipsticks. They’re outdated. Use a blood ketone meter-the same one used for type 1 diabetes. Point-of-care testing should be standard in any ER or urgent care where a diabetic on an SGLT2 inhibitor walks in with nausea or vomiting.
The Cleveland Clinic’s protocol says: if you’re on an SGLT2 inhibitor and you have these symptoms, get your blood ketones tested within 15 minutes of triage. No exceptions. No waiting. No “let’s check glucose first.”

Emergency Treatment: It’s Not the Same as Classic DKA
Treatment follows the same general path as classic DKA: fluids, insulin, electrolytes. But the details matter-because your glucose isn’t high.Fluids: Start with 0.9% saline at 15-20 mL/kg in the first hour. Then keep giving it-250-500 mL/hour-to correct dehydration. But don’t stop just because glucose drops. You need volume.
Insulin: Begin at 0.1 units/kg/hour. But here’s the critical difference: start glucose-containing fluids early. In classic DKA, you wait until glucose is below 250 mg/dL before adding dextrose. In euglycemic DKA, you might need to add 5% or 10% dextrose after the first hour. Why? Because insulin will crash your glucose fast. You don’t want to go from euglycemia to hypoglycemia while fixing acidosis.
Potassium: Total body potassium is almost always low-even if your serum level looks normal. About 65% of patients need aggressive replacement. Check levels every 2 hours. Don’t wait for it to drop.
Monitoring: Track ketones, glucose, and bicarbonate every 1-2 hours. Beta-hydroxybutyrate should drop by 0.5-1.0 mmol/L per hour. If it’s not falling, you may need more insulin or more fluids.
Who’s at Highest Risk?
Not everyone on an SGLT2 inhibitor will get euglycemic DKA. But certain situations raise the risk dramatically:- Illness (infection, flu, COVID-19)
- Surgery or major stress
- Pregnancy
- Drinking alcohol
- Severely cutting carbs or fasting
- Type 1 diabetes (even if off-label)
- Low C-peptide levels (meaning your pancreas makes little insulin)
Patients with type 2 diabetes who have had DKA before, or who have very low insulin production, are especially vulnerable. That’s why the American Association of Clinical Endocrinology recommends not starting SGLT2 inhibitors in anyone with a history of DKA.

How to Prevent It
Prevention is easier than treatment-and it’s all about education and timing.For patients: If you’re on an SGLT2 inhibitor, you need to know:
- Stop taking your drug if you’re sick, having surgery, or can’t eat.
- Check your blood ketones if you feel nauseous, tired, or have stomach pain-even if your glucose is normal.
- Don’t skip meals or go on extreme low-carb diets while on these drugs.
- Call your doctor or go to the ER if ketones are above 1.5 mmol/L.
For providers: Every prescription for an SGLT2 inhibitor should come with a warning card. The FDA now requires that all packaging include this exact language: “Stop taking this medication and seek immediate medical attention if you have symptoms of ketoacidosis, even if your blood sugar is normal.”
Many clinics now use electronic alerts. If a patient is prescribed an SGLT2 inhibitor, their chart flags them for ketone education at every visit. Some add automated texts: “Did you know SGLT2 inhibitors can cause DKA even with normal sugar? Check ketones if you’re sick.”
What’s Changing Now?
Since the FDA’s 2015 warning, awareness has improved. DKA cases linked to SGLT2 inhibitors have dropped by 32%. But here’s the twist: euglycemic DKA now makes up 41% of all SGLT2-related DKA cases-up from 28% in 2015. Why? Because providers are finally checking ketones. The problem isn’t gone. It’s just better identified.Researchers are now testing tools to predict who’s at risk before symptoms start. One 2023 study found that a high ratio of acetoacetate to beta-hydroxybutyrate in the blood can predict euglycemic DKA 24 hours before it hits-with 87% accuracy. Another study is combining HbA1c swings with C-peptide levels to spot high-risk patients with 82% accuracy.
But the real breakthrough isn’t a new test. It’s a mindset shift. As Dr. Kieren Mather told the FDA in 2023: “The key isn’t avoiding these drugs. It’s stopping the false belief that DKA only happens with high sugar.”
Bottom Line
SGLT2 inhibitors are powerful drugs. They help with weight loss, heart protection, and kidney health. But they come with a hidden risk-one that doesn’t show up on your glucose meter.If you’re on one of these drugs, know the signs. If you’re a provider, test ketones first when symptoms appear. Don’t wait for glucose to rise. Don’t assume it’s just a stomach bug. And never let normal blood sugar make you ignore the acid.
Euglycemic DKA kills because it’s invisible. But it doesn’t have to.
Can you get euglycemic DKA if you have type 2 diabetes?
Yes. While SGLT2 inhibitors are approved for type 2 diabetes, they can still trigger euglycemic DKA-even in people who’ve never had DKA before. About 20% of cases occur in type 2 patients with no prior history. The risk is lower than in type 1, but it’s real and often missed because blood sugar looks normal.
Should I stop my SGLT2 inhibitor if I’m sick?
Yes. If you have an infection, fever, vomiting, surgery, or can’t eat for more than a day, stop taking your SGLT2 inhibitor. Resume only after you’re fully recovered and eating normally. Most guidelines recommend holding the drug for at least 24-48 hours during acute illness. Talk to your doctor about when to restart.
Do I need to check ketones if my blood sugar is normal?
Absolutely. If you’re on an SGLT2 inhibitor and feel nauseous, tired, have abdominal pain, or are breathing fast, check your blood ketones-even if your glucose is 120 or 180 mg/dL. A reading above 1.5 mmol/L means you’re at risk for DKA. Go to urgent care or the ER. Don’t wait for symptoms to worsen.
Why don’t doctors always catch euglycemic DKA?
Because the old rule was: DKA = high sugar. That’s what every textbook taught. Even experienced providers were trained to look for glucose above 250 mg/dL. When patients showed up with normal sugar, they assumed it wasn’t DKA. The FDA’s 2015 warning changed that, but many still don’t test ketones unless glucose is high. It’s a cognitive bias-and it’s deadly.
Are there any new tests to predict euglycemic DKA?
Yes. A 2023 study found that a high ratio of acetoacetate to beta-hydroxybutyrate in the blood can predict euglycemic DKA 24 hours before symptoms appear, with 87% accuracy. Another study is using HbA1c variability and C-peptide levels to identify high-risk patients with 82% accuracy. These tools aren’t routine yet, but they’re coming fast.
Can I still take SGLT2 inhibitors if I have type 1 diabetes?
They’re not approved for type 1 diabetes, but some doctors prescribe them off-label for weight or kidney benefits. If you have type 1 and are taking one, your risk of DKA is 5-12%. Experts recommend extreme caution. Only use them if you’re closely monitored, have stable insulin dosing, and understand the risks. Never skip insulin or reduce carbs while on these drugs.
