Dairy Products and Antibiotic Absorption: Why Timing Is Critical

Dec, 9 2025
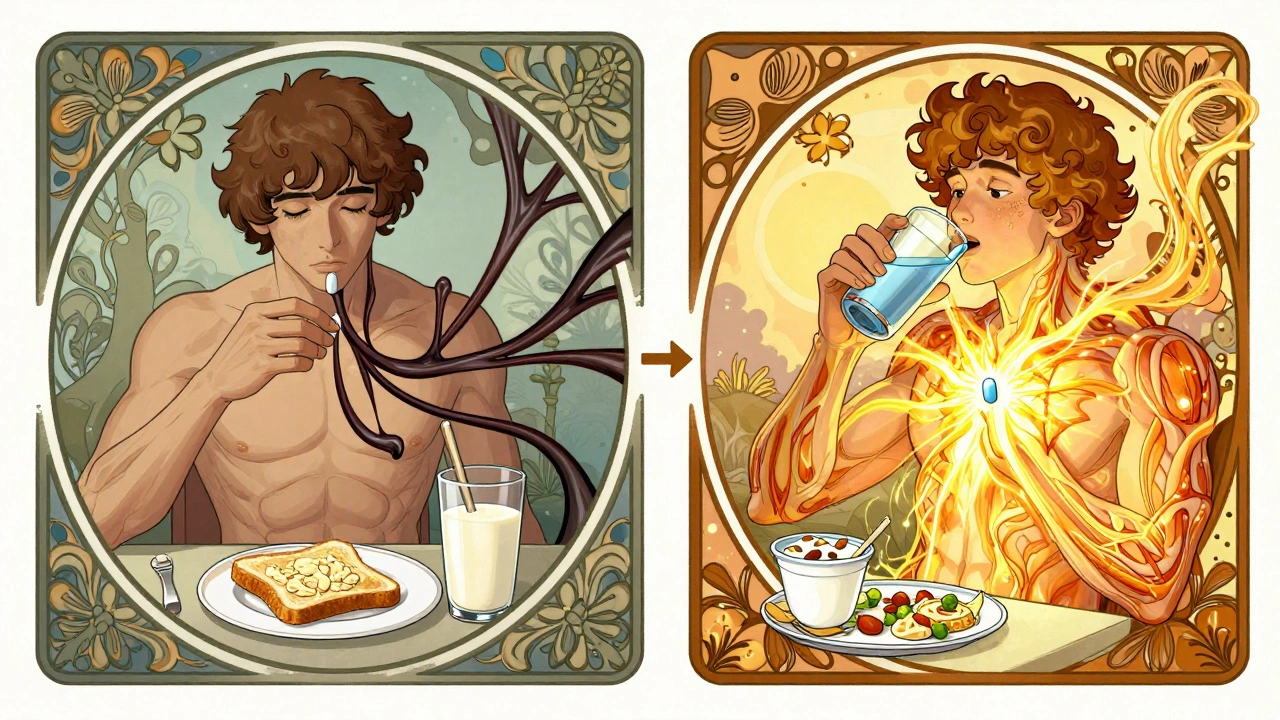
When you’re sick and your doctor prescribes an antibiotic, you want it to work. Not just a little - you want it to kill the infection fast and keep it from coming back. But what if something in your breakfast or dinner is quietly stopping that antibiotic from doing its job? It’s not just a myth. For certain antibiotics, dairy products like milk, cheese, yogurt, and even calcium-fortified plant milks can seriously reduce how well your body absorbs the medicine. And if you don’t know when to avoid them, your treatment could fail - even if you take every pill exactly as directed.
Why Dairy Interferes with Some Antibiotics
The problem isn’t dairy itself. It’s the calcium. And magnesium. And iron. These minerals are naturally found in milk and dairy products, and they bind tightly to certain antibiotics in your stomach and intestines. When they do, they form a kind of chemical cage - an insoluble complex - that your body can’t absorb. That means the antibiotic just passes through you, useless. You think you’re getting the full dose, but your bloodstream might only get 10% of it. This isn’t new science. Researchers first noticed this in the 1960s with tetracycline antibiotics. Since then, dozens of studies have confirmed it. The Journal of Rawal Academy of Sciences found that milk cut ciprofloxacin absorption by 70%, and yogurt dropped it by 92%. That’s not a small drop - that’s treatment failure territory. Your infection doesn’t get treated. It lingers. And when bacteria survive a weak antibiotic dose, they learn to resist it. That’s how antibiotic resistance starts.Which Antibiotics Are Affected?
Not all antibiotics are affected. Penicillin, amoxicillin, azithromycin - these are fine with dairy. But two major classes are high-risk:- Tetracyclines: This group includes tetracycline, doxycycline, and minocycline. Tetracycline is the most sensitive - dairy can block up to 90% of absorption. Doxycycline is a bit more forgiving, but still affected. Studies show even with doxycycline, taking it with milk can cut blood levels by 30-50%.
- Fluoroquinolones: This group includes ciprofloxacin (Cipro), levofloxacin (Levaquin), and moxifloxacin (Avelox). These are commonly prescribed for urinary tract infections, sinus infections, and pneumonia. Ciprofloxacin is especially vulnerable. One study showed yogurt reduced its absorption by 92% - worse than milk.
How Long Should You Wait?
Timing isn’t just a suggestion - it’s medical necessity. The exact window depends on the antibiotic:- For tetracyclines: Take the pill at least 1 hour before eating dairy, or wait 2 hours after. Some experts recommend 3 hours for maximum safety, especially with older tetracycline.
- For fluoroquinolones like ciprofloxacin: Wait 2 hours before dairy, and 4 to 6 hours after. This is stricter because these drugs are more easily blocked. If you take your cipro at 8 a.m., don’t have your yogurt until at least 2 p.m., and avoid milk at dinner.
It’s Not Just Milk
Many people think only dairy milk is the problem. That’s a dangerous mistake. Calcium-fortified orange juice? Same issue. Soy milk, almond milk, oat milk - if they’re fortified with calcium carbonate or calcium phosphate, they’ll bind to your antibiotic just like cow’s milk. A 2023 study in the Journal of the American Pharmacists Association found that 40% of patients didn’t realize plant-based milks could interfere. If the label says “calcium added,” treat it like dairy. Even antacids, multivitamins, and iron supplements can cause the same problem. If you take a daily calcium pill, don’t take it at the same time as your antibiotic. Separate them by at least 2 hours - better yet, take the calcium at bedtime and the antibiotic in the morning.What Happens When You Ignore the Rules?
Real people get sick because of this. On Reddit, a nurse shared a case: a patient on doxycycline for Lyme disease kept having flare-ups. She was taking her pill with breakfast - toast and milk. Once they told her to wait two hours, her symptoms cleared up in days. A Drugs.com user with a recurring UTI had the same story - her infection came back every time she had yogurt after her cipro dose. After switching to a 4-hour gap, it never returned. Studies back this up. A 2023 analysis in the Journal of Patient Experience found that patients who followed the timing rules had a 98% success rate. Those who didn’t? Only 72%. That’s a 26-point gap - the difference between getting better and needing a second round of antibiotics. And it’s not just about one infection. The WHO estimates that improper antibiotic use - including timing errors with dairy - contributes to 5-10% of antibiotic resistance cases in community settings. That means your mistake today could make antibiotics less effective for someone else tomorrow.What About Doxycycline? Is It Safer?
Yes - but not safe enough to ignore. Doxycycline is a newer version of tetracycline, designed to be absorbed more easily. It’s less affected by calcium than its older cousins. Still, studies show it can lose up to 50% of its effectiveness when taken with milk. The GoodRx guidelines say: “In general, it’s a good idea to take oral tetracyclines at least 1 hour before or 2 hours after any dairy products.” Don’t assume you’re immune because your doctor said “doxycycline is better.” It’s better - not bulletproof.
Practical Tips for Real Life
Life isn’t a lab. You’ve got breakfast, lunch, dinner, and snacks. Here’s how to make it work:- Schedule smart: Take your antibiotic first thing in the morning on an empty stomach. Wait two hours before your coffee and toast with butter. Have dairy at lunch or dinner instead.
- Use bedtime wisely: If you take your antibiotic twice a day, take the second dose at bedtime. Skip dairy snacks after dinner. Drink water instead.
- Check labels: Look for “calcium added” on plant milks, juices, and even some protein bars.
- Ask your pharmacist: They see this every day. When you pick up your prescription, ask: “Does this interact with dairy or calcium?” Don’t assume the doctor told you.
- Set phone alerts: Use apps like Medisafe or MyMeds. They can remind you when it’s safe to eat dairy after your dose.
What’s Changing?
The FDA updated labeling rules in January 2023. Now, all tetracycline and fluoroquinolone packages must include clear timing instructions - not just “avoid dairy.” That’s progress. Digital health tools are catching up too. Apps now flag dairy interactions automatically when you log your meds. Pharmaceutical companies are also working on new versions of these antibiotics that resist calcium binding. Early trials show promise, but don’t expect them before 2026. Until then, timing is your only tool.Bottom Line
Dairy doesn’t ruin all antibiotics. But for the ones that matter - the ones you’re prescribed for serious infections - it can sabotage your treatment. It’s not about being perfect. It’s about being smart. Take your antibiotic on an empty stomach. Wait two to six hours before you have cheese, milk, or fortified oat milk. Don’t guess. Don’t assume. Ask your pharmacist. Your body will thank you - and so might the next person who needs the same drug.Can I drink milk with doxycycline if I wait a few hours?
No - you should avoid dairy for at least 2 hours after taking doxycycline. While doxycycline is less affected by calcium than older tetracyclines, studies still show it can lose up to half its effectiveness if taken with milk or cheese. Waiting 2 hours minimizes this risk. For safety, take it on an empty stomach and avoid dairy until after your next meal.
Is yogurt worse than milk for antibiotic absorption?
Yes, yogurt can be worse. A 2022 study in the Journal of Rawal Academy of Sciences found yogurt reduced ciprofloxacin absorption by 92%, compared to 70% for milk. This is likely because yogurt contains higher concentrations of calcium and other minerals, and its thicker texture may slow digestion, giving more time for binding. Even if it’s labeled “low-fat” or “probiotic,” it still interferes.
Can I take my antibiotic with water instead of milk?
Yes - water is the best choice. Avoid juice, coffee, tea, or soda unless you’re sure they’re not calcium-fortified. Some orange juices and plant-based milks are fortified with calcium, and they act just like dairy. Stick to plain water when taking antibiotics like doxycycline or ciprofloxacin.
What if I accidentally take my antibiotic with milk?
Don’t panic - but don’t ignore it either. If you realize within an hour, wait and take another dose only if your doctor or pharmacist says it’s safe. Never double up on your own. If it’s been more than an hour, skip the next dose and resume your schedule. Monitor your symptoms. If your infection doesn’t improve, contact your doctor - you may need a different antibiotic or a longer course.
Do all antibiotics interact with dairy?
No. Antibiotics like amoxicillin, azithromycin, penicillin, and clindamycin are not affected by dairy. But if your prescription ends in “-cycline” or “-floxacin,” assume it is. Always check the label or ask your pharmacist. Never assume your antibiotic is safe - always confirm.
