Herbal Supplements and Drug Interactions: What You Need to Know for Safety
Nov, 27 2025
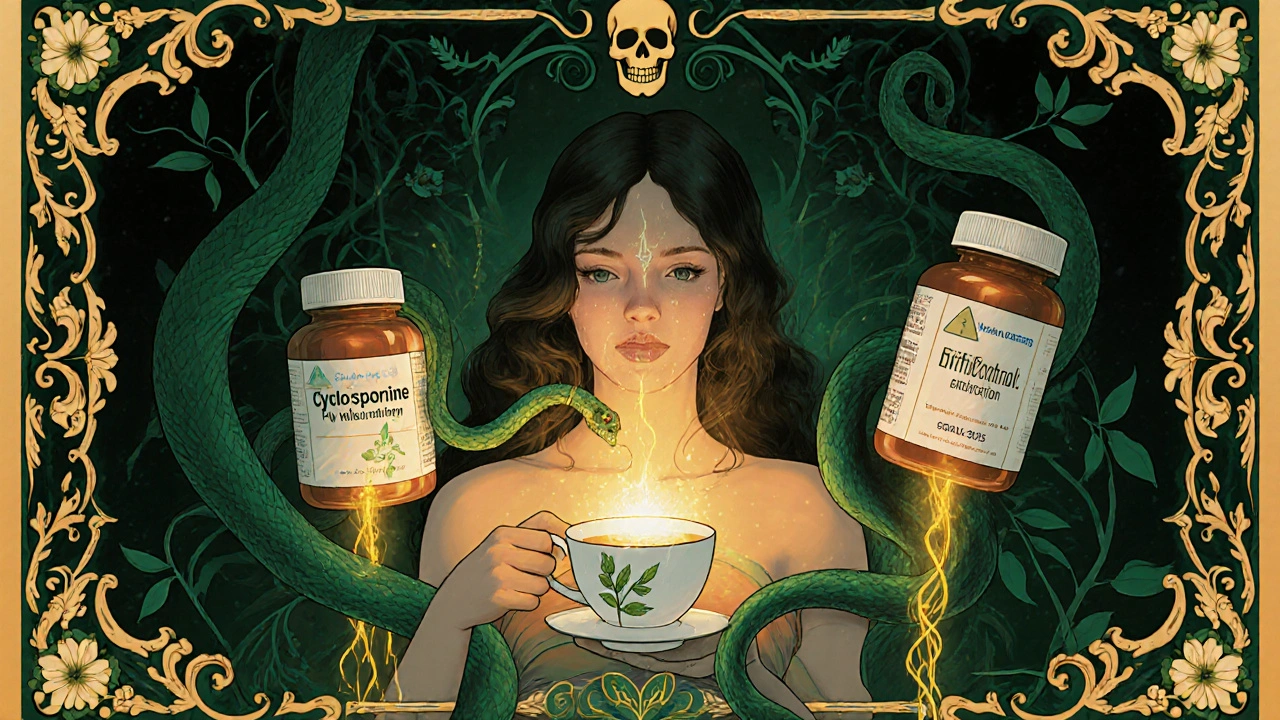
Every year, millions of people take herbal supplements thinking they’re harmless because they’re "natural." But here’s the truth: herbal supplements aren’t harmless. They’re powerful. And when mixed with prescription drugs, they can cause serious, even life-threatening, problems.
Why Herbal Supplements Aren’t Just Tea
People often assume that if something comes from a plant, it’s safe. That’s a dangerous myth. St. John’s wort, ginkgo biloba, garlic, and goldenseal aren’t gentle remedies-they’re bioactive compounds that directly interfere with how your body processes medications. These aren’t just theoretical risks. Real people have had organ transplants fail, strokes happen, and blood thinners turn deadly because they didn’t know their daily tea or capsule was changing how their drugs worked. The science is clear: herbal products affect the same enzymes and transporters in your liver and gut that prescription drugs rely on. The most important of these is the CYP3A4 enzyme, which handles about half of all medications. When you take St. John’s wort, it turns this enzyme into overdrive, flushing drugs out of your system before they can work. That’s why transplant patients on cyclosporine have lost their organs after starting St. John’s wort. It’s not magic. It’s biochemistry.St. John’s Wort: The King of Dangerous Interactions
If you’re on any prescription medication, St. John’s wort is the one herb you need to avoid unless your doctor says it’s okay. This supplement, often taken for mild depression, is the most dangerous herbal product on the market when mixed with drugs. It reduces blood levels of:- Cyclosporine by up to 57% - leading to organ rejection
- Digoxin by 25% - causing heart rhythm problems
- Oral contraceptives - resulting in unplanned pregnancies
- HIV protease inhibitors by 40-80% - allowing the virus to rebound
Ginkgo Biloba and the Silent Bleeding Risk
Ginkgo biloba is popular for memory and circulation. But if you’re on warfarin, aspirin, clopidogrel, or any blood thinner, you’re playing Russian roulette. Ginkgo inhibits platelets, making your blood less likely to clot. When combined with anticoagulants, the risk of dangerous bleeding increases by about 30%. That’s not a small bump. That’s a spike into emergency room territory. Doctors in Australia and the U.S. have reported cases where patients had unexplained bruising, nosebleeds, or brain bleeds after starting ginkgo. One hematologist in Adelaide saw three cases in a single year-all patients had stopped mentioning their ginkgo supplements during checkups. They didn’t think it mattered.Garlic, Goldenseal, and the Hidden Metabolism Saboteurs
Garlic supplements are often taken for heart health. But they can slash saquinavir (an HIV drug) levels by 51%. That’s not a typo. It’s a treatment failure. Goldenseal is even more dangerous. It blocks the CYP3A4 and CYP2D6 enzymes, which means drugs like metoprolol (for high blood pressure), dextromethorphan (in cough syrup), and even some antidepressants build up in your blood to toxic levels. One study showed dextromethorphan levels rising by 50%-enough to cause hallucinations, seizures, or respiratory failure. These aren’t rare cases. They’re predictable. And they’re avoidable-if you tell your doctor.
Other High-Risk Herbs You Might Not Know About
- Danshen (Salvia miltiorrhiza): Used in traditional Chinese medicine for heart health. But it increases the risk of irregular heartbeat by 35% when taken with digoxin. That’s not just a side effect-it’s a cardiac emergency waiting to happen. - Hawthorn: Marketed for blood pressure and heart support. When combined with beta-blockers or digoxin, it can drop systolic pressure below 90 mmHg, leading to dizziness, fainting, or cardiac arrest. - American Ginseng: Many assume it’s safe. But it can reduce warfarin’s effect by mimicking vitamin K. One patient’s INR dropped from 4.9 to 1.9 in just two weeks after starting ginseng. That’s the difference between protection and stroke. - Valerian: Often used for sleep. It can make benzodiazepines like lorazepam or diazepam too strong, causing extreme drowsiness, slowed breathing, or coma.Why Doctors Don’t Always Know
Here’s the ugly truth: most doctors don’t ask about herbal supplements. And most patients don’t volunteer the information. A 2016 study found that 72% of hospital patients taking herbal products weren’t even known to their care team. Why? Because patients think: "It’s just a supplement." Or: "My doctor didn’t ask." Or: "It’s natural, so it’s fine." A 2022 Consumer Reports survey showed 68% of supplement users never told their doctor. That’s not ignorance-it’s a systemic failure. The medical system treats supplements like harmless snacks, not drugs. But they’re not.What You Should Do Right Now
If you take any prescription medication and any herbal product-even if you’ve been doing it for years-here’s what to do:- Make a list of every supplement you take: name, dose, how often.
- Include teas, tinctures, and powders-not just pills.
- Take that list to your doctor or pharmacist.
- Ask: "Could any of these interact with my medications?" Don’t say "Is this safe?" Say "Could this make my drugs stop working or become too strong?"

What the System Isn’t Telling You
In the U.S., the FDA doesn’t require supplement makers to prove their products are safe before selling them. The 1994 Dietary Supplement Health and Education Act (DSHEA) lets companies sell anything labeled as a "dietary supplement" without testing for interactions. There are over 23,000 herbal supplement products on the U.S. market. Only 15% include any warning about drug interactions. And the FDA issued just 12 warning letters about interaction risks in 2022-despite monitoring over 80,000 products. That’s not oversight. That’s negligence.How to Talk to Your Pharmacist
Pharmacists are your best defense. They’re trained to spot interactions. But they can’t help if they don’t know what you’re taking. Bring your supplements to the pharmacy-not just a list. Show them the bottles. Ask: "Could this cause problems with my blood pressure meds? My heart pill? My antidepressant?" A 2021 study showed that when pharmacists used visual aids-photos of common herbal products-patients were 47% more likely to admit to using them. Pictures break the silence.What’s Being Done About It
There’s progress. The NIH spent $12.7 million in 2023 just to study herb-drug interactions. The FDA is drafting new rules to require interaction testing for new botanical drugs. The European Medicines Agency now requires full interaction studies for herbal medicines sold as drugs. A new AI tool from the University of California can predict unknown interactions with 87% accuracy by analyzing 3,000+ known cases. But these tools won’t save you unless you speak up.Final Reality Check
"Natural" doesn’t mean safe. "Herbal" doesn’t mean gentle. And not telling your doctor about your supplements isn’t privacy-it’s putting your life at risk. St. John’s wort isn’t a tea. It’s a drug. Ginkgo isn’t a memory booster. It’s a blood thinner. Goldenseal isn’t a cold remedy. It’s a metabolic saboteur. You wouldn’t mix two prescription pills without asking your doctor. Don’t mix a supplement with your pills either. Your health isn’t a guessing game. It’s a partnership. And you need to bring all the facts to the table.Can herbal supplements really make my prescription drugs stop working?
Yes. St. John’s wort is the most well-documented example. It can reduce the blood levels of cyclosporine by 57%, digoxin by 25%, and HIV medications by up to 80%. This isn’t theoretical-it’s led to organ rejection, HIV treatment failure, and unplanned pregnancies. Many other herbs, like garlic and ginseng, also interfere with how your body absorbs or breaks down drugs.
I’ve been taking ginkgo biloba for years with my blood thinner. Should I stop?
Stop taking it immediately and call your doctor. Ginkgo increases bleeding risk by about 30% when combined with warfarin or aspirin. Even if you haven’t had problems yet, the risk builds over time. Many bleeding events happen suddenly, with no warning. Your INR levels may look normal, but ginkgo can still be silently thinning your blood. Don’t wait for symptoms.
Are supplements labeled as "drug-free" safe to take with my medications?
No. The term "drug-free" on a supplement label only means it doesn’t contain synthetic pharmaceuticals. It says nothing about the herbal ingredients’ biological activity. St. John’s wort, ginkgo, and goldenseal are all natural-and all interact with drugs. Labels are not regulated for interaction warnings. Assume every herbal product can affect your meds unless proven otherwise.
Why don’t my doctors ask about supplements?
Most doctors aren’t trained to ask. Medical schools rarely include herbal interactions in their curriculum. And many assume patients won’t volunteer the information because they think supplements are harmless. A 2024 review found only 3% of primary care providers routinely screen for herbal use. Don’t wait for them to ask-bring it up yourself. Use the exact words: "I take [name of supplement]. Could it interfere with my [medication]?"
Is there a safe herbal supplement I can take with my heart medication?
There’s no blanket answer. Even herbs considered "low risk," like milk thistle or saw palmetto, haven’t been studied enough in people on heart drugs. Hawthorn, often used for heart health, can dangerously lower blood pressure when combined with beta-blockers. The only safe approach is to show your doctor every supplement you take and ask: "Is this safe with my current meds?" Never assume safety. Always verify.
