Microscopic Colitis: Understanding Chronic Diarrhea and Why Budesonide Is the First-Line Treatment
Jan, 30 2026
What Is Microscopic Colitis?
Microscopic colitis is a hidden cause of long-lasting, watery diarrhea that doesn’t show up on a regular colonoscopy. You can look at your colon with an endoscope, and everything appears normal-no ulcers, no swelling, no bleeding. But when a doctor takes a tiny tissue sample and looks at it under a microscope, they see inflammation. That’s the whole point: the damage is microscopic.
There are two types: collagenous colitis and lymphocytic colitis. In collagenous colitis, a thick band of collagen forms just below the surface of the colon lining, blocking water absorption. In lymphocytic colitis, there’s a flood of immune cells (lymphocytes) inside the lining. Both lead to the same problem: your colon can’t hold onto water, so you have frequent, watery stools-often 5 to 10 times a day.
This condition mostly hits people over 50, and women are more likely to get it than men. It’s not contagious. It’s not caused by food poisoning. And it’s not Crohn’s disease or ulcerative colitis, even though it’s grouped under inflammatory bowel diseases. The key difference? Those other conditions show visible damage on scans. Microscopic colitis hides in plain sight.
Why Do People With Microscopic Colitis Have Constant Diarrhea?
The diarrhea isn’t just annoying-it’s life-changing. People describe it as sudden, urgent, and relentless. Many wake up at night needing to go. Some can’t leave the house without knowing where every bathroom is. Weight loss is common, especially in collagenous colitis. Fecal incontinence happens in about a third of cases.
Abdominal pain isn’t always present, but when it is, it’s usually crampy and comes and goes. Unlike infections that clear up in days, microscopic colitis drags on. Most people suffer for months, sometimes years, before getting a diagnosis. The average time from first symptom to confirmed diagnosis? Eleven months.
Why so long? Because doctors don’t always think of it. Routine tests like stool cultures and blood work come back normal. Colonoscopies look fine. Only when biopsies are taken from the right spots-usually the right side of the colon-and examined under high magnification can the diagnosis be made. Many patients are misdiagnosed with IBS until a biopsy finally reveals the truth.
Why Budesonide Is the Go-To Treatment
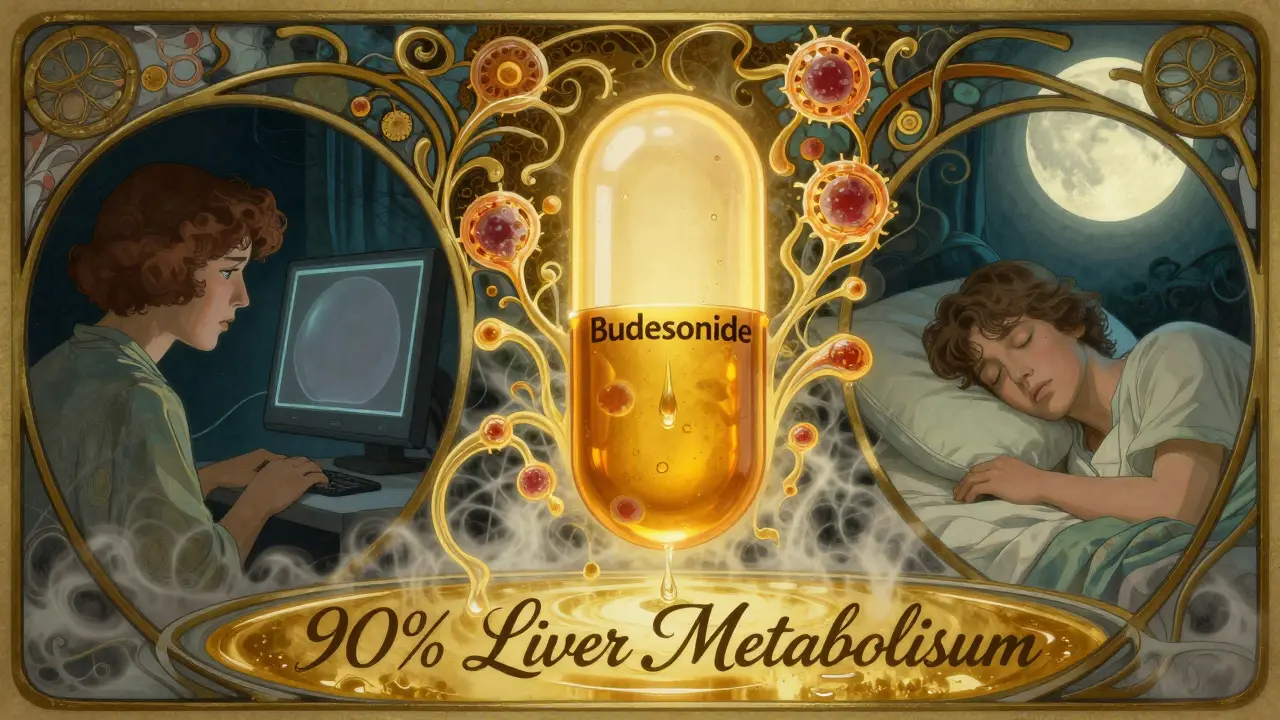
When you have moderate to severe microscopic colitis-meaning you’re having four or more watery stools a day-budesonide is the first drug doctors reach for. It’s not a regular steroid like prednisone. It’s designed to work right in the gut and then get broken down by the liver before it can affect the rest of your body.
That’s why it’s so much safer. About 90% of budesonide is metabolized on its first pass through the liver. Only 10-15% enters your bloodstream. Compare that to prednisone, which floods your whole system. With prednisone, you risk high blood sugar, bone thinning, insomnia, and mood swings. With budesonide, side effects are mild: maybe some acne, trouble sleeping, or a bit of moodiness. Serious side effects are rare.
Studies show that 75-85% of people with microscopic colitis go into remission within 6 to 8 weeks of taking 9 mg of budesonide daily. That’s a huge jump from the 25-30% who improve on a placebo. In one major trial, 84% of collagenous colitis patients had their diarrhea stop completely after eight weeks. For many, it’s the first time in years they’ve slept through the night.
How Budesonide Works and How It’s Taken
Budesonide is usually taken as a capsule, once a day in the morning. The standard dose is 9 mg for 6 to 8 weeks. Most people start feeling better within 10 days. By week 4, 70-80% are significantly improved. It doesn’t cure the disease-it controls it. That’s an important distinction.
After the initial course, symptoms often come back. About half of patients relapse within a year after stopping. That’s why maintenance therapy is common. Some people stay on 6 mg daily for months or even years. Others try to taper down slowly-cutting the dose by 3 mg every few weeks-to see if they can stay off it.
There’s no one-size-fits-all plan. If symptoms return after stopping, restarting budesonide usually works again. Some patients need long-term low-dose therapy. Others find they can manage with diet changes or other meds after one or two courses.
What About Other Treatments?
Budesonide isn’t the only option, but it’s the most effective. Other drugs fall short.
- Bismuth subsalicylate (Pepto-Bismol) helps about 26% of people. It’s cheap and safe, but not strong enough for severe cases.
- Mesalamine (Asacol) works in 40-50% of cases. It’s often tried if budesonide isn’t an option, but it’s less reliable.
- Cholestyramine helps if bile acid malabsorption is part of the problem-which it often is. Up to 70% of patients improve with this powder, especially when combined with budesonide.
- Prednisone works just as well as budesonide, but the side effects make it a last resort. About 45% of people on prednisone have problems like high blood sugar or bone loss. Only 15% on budesonide do.
- Biologics like infliximab are expensive ($2,500-$3,000 per infusion) and only help 20-30% of patients. They’re reserved for those who don’t respond to anything else.
Combination therapy is becoming more common. For example, taking budesonide with cholestyramine can fix diarrhea completely in patients who’ve suffered for years. One Reddit user wrote, “After three years of misery, budesonide + bile binder finally gave me back my life.”
Cost, Access, and Real-World Challenges
Generic budesonide became available in 2018, and prices dropped by 60%. Now, an 8-week course costs $150-$250. The branded version, Entocort EC, still runs $800-$1,200. Insurance usually covers it, but without coverage, many patients can’t afford it.
Even when people get the drug, tapering off is tricky. About 65% of patients say it’s hard to reduce the dose without symptoms returning. Doctors need to be patient and adjust slowly. The Crohn’s & Colitis Foundation recommends dropping the dose by 3 mg every 2-4 weeks.
Long-term use raises questions. We don’t have solid data on adrenal suppression in older adults after more than a year of daily budesonide. That’s why doctors check bone density, blood sugar, and blood pressure before starting-and monitor them yearly if you’re on maintenance therapy.
What’s Next for Microscopic Colitis?
Research is moving fast. In 2023, the FDA gave fast-track status to vedolizumab, a biologic that targets gut-specific immune cells. Early results show 65% remission at 14 weeks-better than most current options. If approved, it could become a new option for people who relapse on budesonide.
Scientists are also looking at genetics. The COLMICS trial found that people with certain immune genes (HLA-DQ2/DQ8) respond better to budesonide. That could mean future testing to predict who will benefit most.
Another change on the horizon? Using fecal calprotectin to track inflammation without repeated biopsies. If levels drop below 50 μg/g, it’s a good sign treatment is working. This test could make monitoring easier and cheaper.
Final Thoughts: Is Budesonide Right for You?
If you’ve had chronic, watery diarrhea for months and no one can explain why, microscopic colitis might be the answer. Ask your doctor for biopsies during your colonoscopy-even if everything looks normal. That’s the only way to know for sure.
If you’re diagnosed, budesonide is your best bet. It’s safe, effective, and backed by strong evidence. It won’t fix everything, and relapses are common, but for most people, it’s life-changing. You don’t need to keep living with 10 bathroom trips a day. Treatment works. You just need to start with the right test and the right drug.
Don’t give up. Many people feel hopeless for years before getting diagnosed. But with the right approach, relief is possible-and it often comes faster than you think.
Can microscopic colitis be cured?
There’s no permanent cure for microscopic colitis, but most people achieve long-term symptom control. Many go into remission with budesonide and stay symptom-free for months or years. Some can stop treatment entirely after one course. Others need maintenance therapy. The goal isn’t a cure-it’s managing the condition so it doesn’t disrupt daily life.
Is budesonide a steroid? Is it safe for long-term use?
Yes, budesonide is a corticosteroid, but it’s designed to act locally in the gut and be broken down quickly by the liver. This means very little enters your bloodstream, making it far safer than older steroids like prednisone. For most people, short-term use (6-8 weeks) has minimal side effects. Long-term use (over a year) is common for relapsing cases, and while we don’t have decades of data, studies show adrenal suppression is rare when used at low maintenance doses. Regular monitoring of bone density and blood sugar is recommended for patients on long-term therapy.
Why do I need a colonoscopy with biopsies if my symptoms are typical?
Because microscopic colitis looks exactly like irritable bowel syndrome (IBS) on the surface. Both cause chronic watery diarrhea. But IBS doesn’t involve inflammation, and it won’t respond to steroids. If you take budesonide without knowing you have microscopic colitis, you might not get better-and you’ll waste time. Biopsies are the only way to confirm the diagnosis. Even if your colon looks normal during the scope, you still need tissue samples taken from the right areas to see the microscopic changes.
Can diet help with microscopic colitis?
Diet won’t cure it, but it can help manage symptoms. Many people find relief by avoiding caffeine, dairy, artificial sweeteners, and high-fat foods. A low-FODMAP diet may reduce bloating and urgency. If bile acid malabsorption is involved (common in microscopic colitis), a low-fat diet and cholestyramine work well together. Some patients benefit from gluten-free diets, especially if they also have celiac disease, which overlaps with microscopic colitis in about 10-15% of cases. But diet alone rarely controls moderate-to-severe diarrhea. Medication like budesonide is still needed.
How do I know if my treatment is working?
You’ll know within 10 to 14 days. If you were having 10 bowel movements a day and now you’re down to 2-3, and they’re less urgent and not watery, the treatment is working. Your doctor may also check your fecal calprotectin level-a marker of gut inflammation. A drop below 50 μg/g suggests improvement. If symptoms don’t improve after 4 weeks, your doctor may adjust your dose or consider other causes.
What happens if budesonide doesn’t work?
If you don’t respond to budesonide after 8 weeks, your doctor will check if the diagnosis is correct. Sometimes biopsies were missed or misread. If the diagnosis is confirmed, other options include cholestyramine, mesalamine, or bismuth subsalicylate. For persistent cases, newer biologics like vedolizumab are being studied and may become available soon. In rare cases, infliximab is used, but it’s expensive and carries risks. Working with a specialist in inflammatory bowel disease is key when first-line treatments fail.
