ACE Inhibitors in Pregnancy: Risks, Alternatives, and What You Need to Know
When you're pregnant and have high blood pressure, choosing the right medication isn't just about controlling numbers—it's about protecting your baby. ACE inhibitors, a class of blood pressure drugs that block angiotensin-converting enzyme to relax blood vessels. Also known as angiotensin-converting enzyme inhibitors, they're commonly used for hypertension, heart failure, and kidney protection in non-pregnant adults. But during pregnancy, they're not just discouraged—they're dangerous. The risks aren't theoretical. Studies show that taking ACE inhibitors during the second and third trimesters can cause serious harm to the developing fetus, including low amniotic fluid, kidney failure, underdeveloped lungs, skull deformities, and even fetal death.
Why does this happen? ACE inhibitors interfere with the renin-angiotensin-aldosterone system, which is critical for fetal kidney development and blood flow. When this system is suppressed, the baby's kidneys can't produce enough urine, leading to oligohydramnios—a dangerous drop in amniotic fluid. This fluid cushions the baby and helps lungs develop. Without it, physical deformities and organ damage can occur. Even if you only took an ACE inhibitor in the first trimester, it's important to tell your doctor. While the risk is lower then, there's still potential for harm, and switching medications early can make a big difference.
So what can you take instead? Labetalol, a beta blocker often used as a first-line treatment for high blood pressure during pregnancy is one of the safest and most common choices. Nifedipine, a calcium channel blocker that relaxes blood vessels without affecting fetal development is another well-studied option. Methyldopa, used for decades, remains a reliable choice too. Your doctor will pick the best fit based on your blood pressure levels, other health conditions, and how far along you are. The goal isn't just to lower numbers—it's to keep you and your baby safe without causing new problems.
Many women don’t realize they’re on an ACE inhibitor until they find out they’re pregnant. If you're taking one for kidney disease or diabetes, talk to your provider before trying to conceive. Switching medications ahead of time gives your body time to adjust and reduces risk. Don’t stop your medication cold—sudden drops in blood pressure can be just as risky as high numbers. Work with your team to make a smooth, safe transition.
You’ll find real stories and detailed comparisons below—what doctors actually recommend, how different drugs affect pregnancy outcomes, and what to do if you’ve already taken an ACE inhibitor. This isn’t about fear—it’s about clarity. You deserve to know what’s safe, what’s not, and what your options really are.
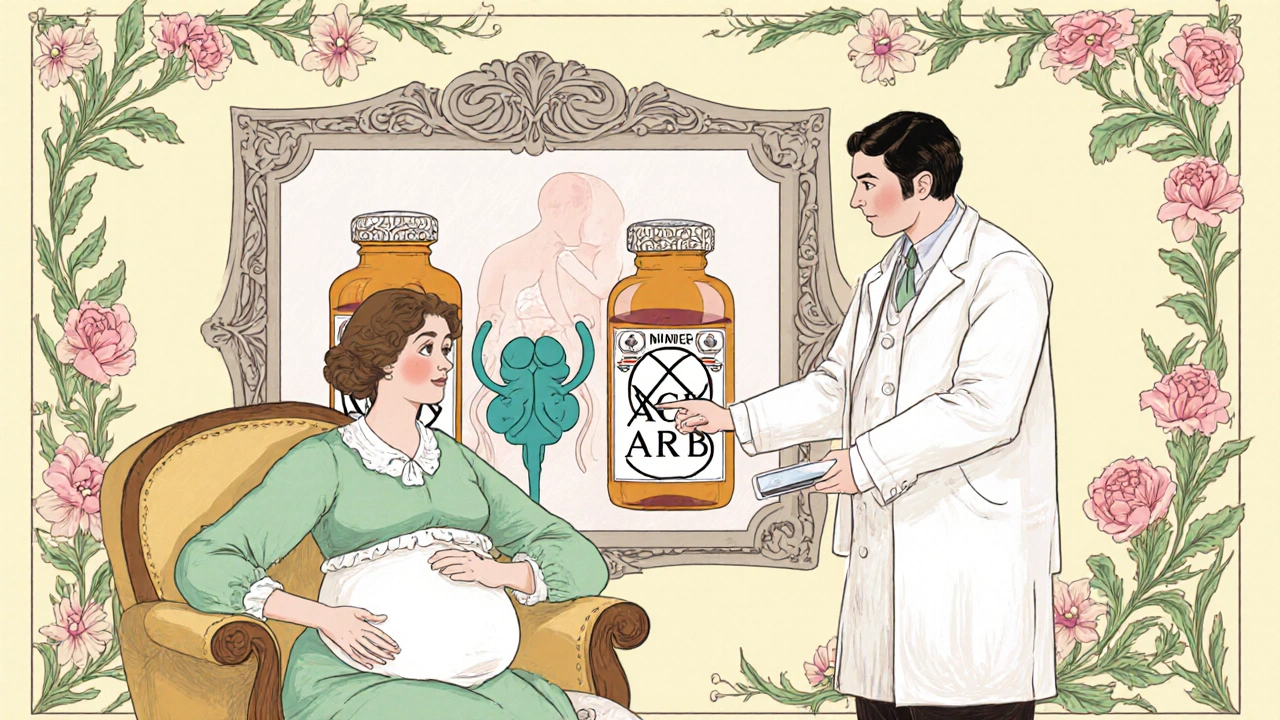
Pregnancy Risks of ACE Inhibitors & ARBs and Safer Alternatives
Caspian Mortensen Oct, 26 2025 8Learn why ACE inhibitors and ARBs are dangerous in pregnancy, see the real fetal risks, and discover safe antihypertensive alternatives with step‑by‑step switching guidance.
More Detail