Understanding Lymphoblastic Leukemia: A Simple Guide
If you or a loved one has been told they have lymphoblastic leukemia, it can feel overwhelming. Let’s break down the basics so you know what’s happening inside the body and what steps come next.
What Is Lymphoblastic Leukemia?
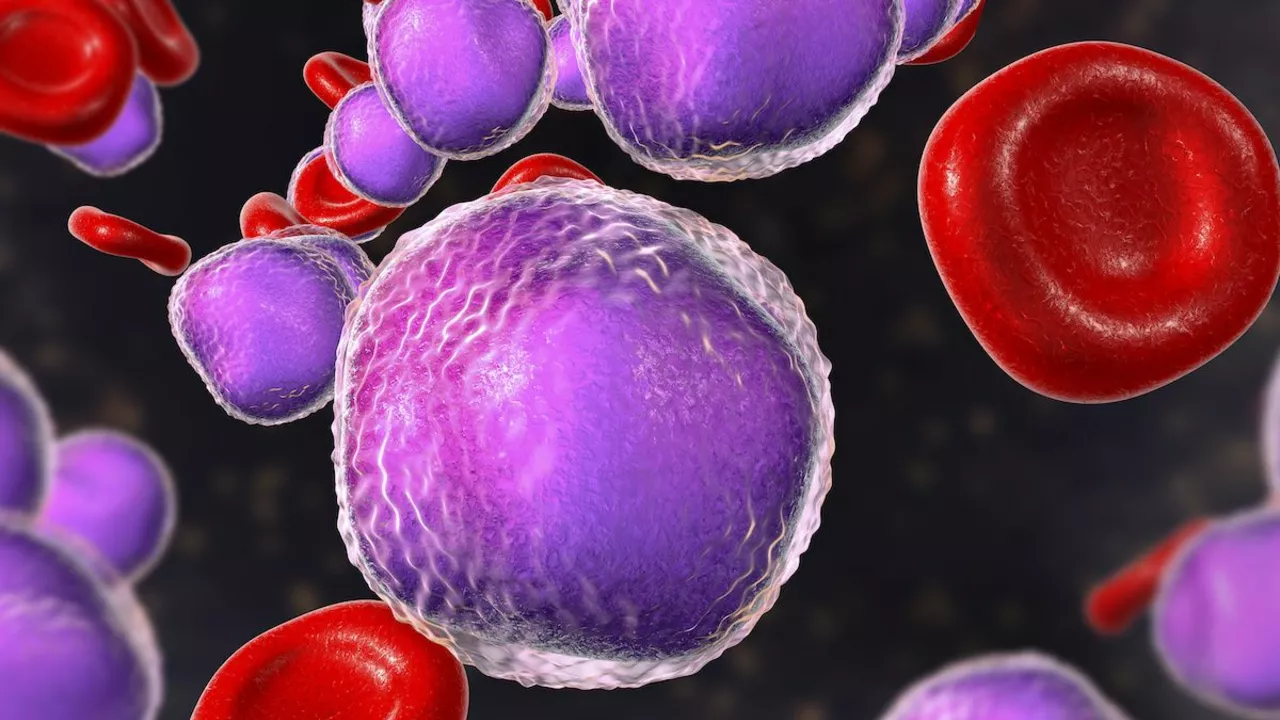
Lymphoblastic leukemia, often called acute lymphoblastic leukemia (ALL), is a cancer of the blood‑forming cells in the bone marrow. It starts when immature white blood cells, called lymphoblasts, grow out of control instead of maturing into normal immune cells. These extra cells crowd out healthy blood cells, leading to fatigue, infections and bleeding problems.
ALL can affect children and adults, but it’s most common in kids under 15. In younger patients the disease tends to respond well to treatment, while older adults may need more intensive therapy.
Symptoms & Diagnosis
The first signs are often vague: tiredness, easy bruising, fever or frequent infections. Because these symptoms match many everyday illnesses, doctors usually run a few quick tests when they suspect leukemia.
A complete blood count (CBC) shows abnormal numbers of white cells, low red cells and platelets. If the CBC looks off, a bone‑marrow aspirate confirms the diagnosis by checking for excess lymphoblasts under a microscope.
Genetic tests are also part of modern work‑ups. Certain chromosome changes, like the Philadelphia chromosome, affect which drugs work best and help doctors estimate prognosis.
Treatment Options
The main goal is to kill leukemia cells and restore normal blood production. Treatment usually happens in phases:
- Induction therapy: a combination of chemotherapy drugs given for several weeks to achieve remission (no detectable cancer).
- Consolidation/Intensification: more chemo or targeted drugs to wipe out hidden cells.
- Maintenance: lower‑dose chemo taken for 1–2 years to keep the disease from coming back.
For patients with specific genetic markers, targeted therapies like tyrosine‑kinase inhibitors (e.g., imatinib) are added. Some children and high‑risk adults may also receive a bone‑marrow or stem‑cell transplant after consolidation.
Side effects can be tough—nausea, hair loss, low immunity—but supportive care (anti‑nausea meds, antibiotics, growth factors) helps manage them. Talk to your oncologist about each drug’s risk profile so you know what to expect.
Living With Lymphoblastic Leukemia
Beyond medical treatment, everyday life matters. Keep a balanced diet, stay hydrated and get gentle exercise when cleared by the doctor. Emotional support is key—join a patient group, talk with a counselor or lean on family.
Regular follow‑up visits track blood counts and catch any signs of relapse early. Most people who finish treatment stay cancer‑free for years, especially children treated on modern protocols.
Knowing what lymphoblastic leukemia looks like, how it’s diagnosed and the steps doctors take can turn fear into action. Stay informed, ask questions, and work with your care team to choose the best plan for you or your loved one.
The Importance of Regular Check-Ups for Chromosome-Positive Lymphoblastic Leukemia Patients
Caspian Mortensen Jun, 26 2023 8As a Chromosome-Positive Lymphoblastic Leukemia patient, I cannot stress enough the importance of regular check-ups. These appointments are crucial for monitoring the progress of the disease, adjusting treatments if necessary, and ensuring early detection of any complications. In addition, regular check-ups also help my healthcare team to stay informed about my overall health and well-being. Moreover, these visits provide an opportunity for me to discuss any concerns or questions I may have with my doctors, fostering a strong and supportive patient-doctor relationship. Ultimately, maintaining a consistent check-up routine is essential for the best possible outcome in managing and fighting this disease.
More Detail