Why Early Detection of Pulmonary Arterial Hypertension Saves Lives

Oct, 3 2025
PAH Risk Assessment Tool
Risk Assessment Result
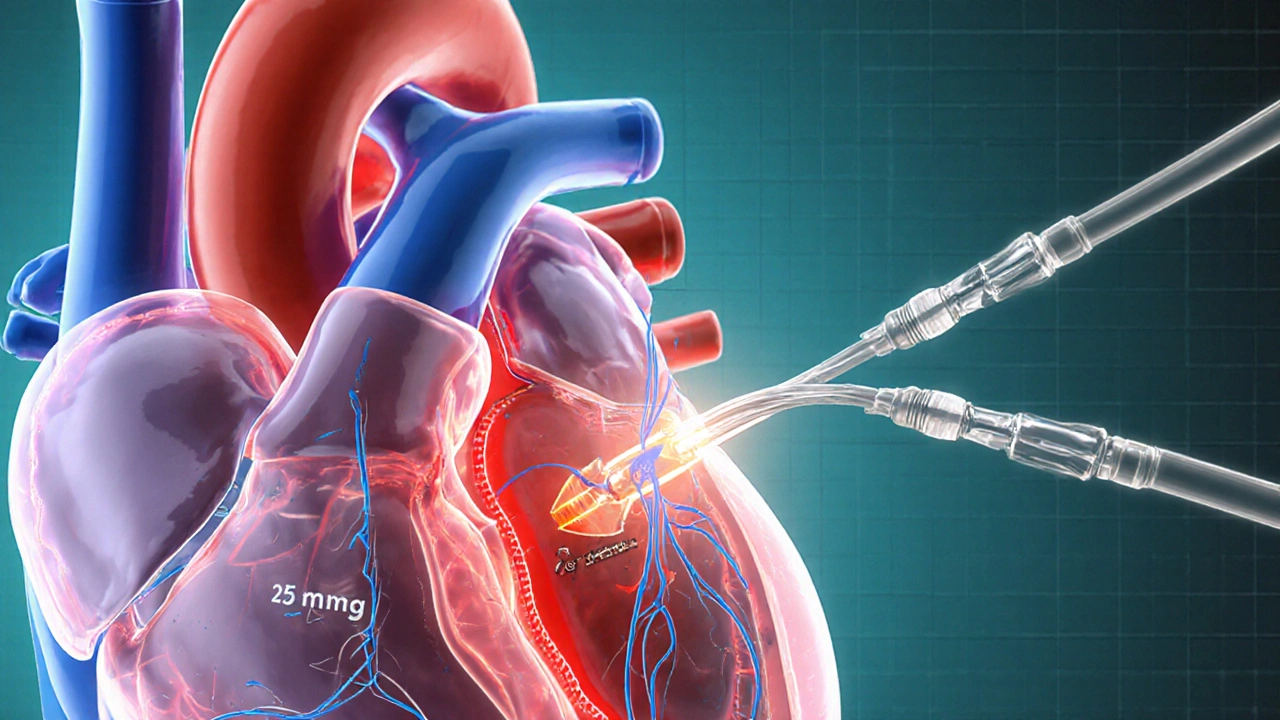
Pulmonary arterial hypertension is a rare, progressive disease that narrows the arteries carrying blood from the heart to the lungs. When pressure in these vessels climbs above 25 mmHg at rest, the right side of the heart must work harder, eventually leading to failure. Because the condition develops slowly, most patients don’t notice anything wrong until the disease is already advanced. Catching it early changes everything - you get more treatment options, better quality of life, and a longer life span.
Quick Takeaways
- Early detection can improve five‑year survival from 40% to over 80%.
- Typical early clues include unexplained shortness of breath on mild activity and subtle fatigue.
- Echo screening and right‑heart catheterisation are the gold‑standard diagnostic steps.
- Patients with a family history or connective‑tissue disease should be screened annually.
- Starting therapy at WHO functional classII, rather than III or IV, dramatically lowers hospitalisation risk.
Why Early Detection Matters
When PAH is diagnosed at an early stage (WHO functional classI‑II), the heart’s right ventricle is still coping relatively well. Studies published in 2023‑2024 show that patients started on combination therapy within the first year of diagnosis have a median time to clinical worsening of 5.2years, compared with just 2.1years for those diagnosed late.
In practical terms, early detection means you can:
- Begin vasodilator therapy before irreversible right‑ventricular remodeling occurs.
- Participate in clinical trials that often exclude classIII/IV patients.
- Maintain a more active lifestyle - the six‑minute walk test (6MWD) is usually >450m in early disease versus <250m later.
- Avoid emergency hospital admissions, which account for 30% of PAH‑related costs.
Recognising the Earliest Signs
PAH doesn’t announce itself with a dramatic chest pain. Instead, watch for these subtle patterns:
- Shortness of breath on climbing a single flight of stairs or brisk walking.
- Unexplained fatigue that isn’t relieved by rest.
- Light‑headedness or faint spells, especially after exertion.
- Swelling in the ankles that appears suddenly.
- Chest discomfort that feels like pressure rather than sharp pain.
If any of these appear and persist for more than a month, a simple echocardiogram can rule out many other heart or lung conditions and flag the possibility of PAH.
The Diagnostic Pathway
Early detection hinges on a step‑wise, evidence‑based work‑up.
- Transthoracic echocardiogram - This non‑invasive scan estimates pulmonary artery pressure and looks for right‑ventricular enlargement. In 2024, a screening protocol using a tricuspid regurgitation velocity >2.8m/s captured 92% of early PAH cases.
- Right‑heart catheterisation - The definitive test. It directly measures mean pulmonary artery pressure, pulmonary capillary wedge pressure, and cardiac output. A mean pressure ≥25mmHg with normal wedge pressure confirms PAH.
- Blood work for biomarkers - Elevated brain natriuretic peptide (BNP) or N‑terminal pro‑BNP often precede overt symptoms.
- Genetic testing - Mutations in the BMPR2 gene are present in ~20% of idiopathic PAH patients. Knowing a patient’s genetic status can trigger earlier screening of relatives.
- Six‑minute walk test (6MWD) - Provides a baseline functional capacity that guides therapy intensity.
Benefits of Starting Treatment Early
Once PAH is confirmed, the therapeutic armamentarium includes endothelin‑receptor antagonists, phosphodiesterase‑5 inhibitors, and prostacyclin analogues. When started at WHO functional classII, combination therapy can:
- Reduce mean pulmonary artery pressure by 10‑15mmHg within 3months.
- Increase 6MWD by an average of 80m, translating into daily activities like gardening or walking the dog.
- Lower the three‑year mortality risk from 45% to under 15% (data from the 2025 REVEAL‑2 registry).
Late‑stage treatment, by contrast, often requires high‑dose intravenous prostacyclin, carries a higher infection risk, and still can’t fully reverse right‑ventricular damage.
Who Should Be Screened?
Guidelines from the European Society of Cardiology (ESC) and the American Heart Association (AHA) recommend targeted screening for high‑risk groups:
- First‑degree relatives of confirmed PAH patients.
- Individuals with connective‑tissue diseases (scleroderma, systemic lupus).
- People with congenital heart disease that leads to increased pulmonary flow.
- Patients with portal hypertension or HIV infection.
For these groups, an annual echo plus BNP check is enough to catch early pressure rises before symptoms appear.
Practical Checklist for Patients and Clinicians
| Metric | Early Detection (ClassI‑II) | Late Detection (ClassIII‑IV) |
|---|---|---|
| 5‑year survival | ≈82% | ≈38% |
| Median time to clinical worsening | 5.2years | 2.1years |
| Average 6MWD improvement after therapy | +80m | +30m |
| Hospitalisation rate (per 100patient‑years) | 12 | 38 |
Use this table as a conversation starter with your doctor. If your numbers align more with the “Late Detection” column, ask about a fast‑track referral to a PAH centre.
Next Steps If You Suspect PAH
- Schedule a transthoracic echocardiogram with a cardiologist experienced in pulmonary hypertension.
- Ask for a right‑heart catheterisation if the echo suggests elevated pressures.
- Discuss genetic testing if you have a family history.
- Begin lifestyle adjustments - low‑sodium diet, moderate aerobic activity, and smoking cessation.
- Enroll in a patient‑support program; many national societies offer free counseling and medication assistance.
Remember, catching PAH early isn’t just about statistics - it’s about staying able to play with your kids, travel, and enjoy everyday moments without the looming fear of a sudden health crisis.
Frequently Asked Questions
What age group is most affected by pulmonary arterial hypertension?
PAH can appear at any age, but it most commonly diagnoses between 30 and 60 years. Younger patients often have a genetic component, while older adults may develop PAH secondary to other conditions like connective‑tissue disease.
Can lifestyle changes delay the need for medication?
Exercise, a low‑salt diet, and avoiding high altitudes can improve symptoms and reduce strain on the right ventricle, but they don’t replace approved PAH therapies. Early medication combined with a healthy lifestyle offers the best prognosis.
How often should high‑risk individuals be screened?
Annual transthoracic echocardiography with BNP testing is recommended for first‑degree relatives of PAH patients, those with scleroderma, and individuals with congenital heart defects that affect pulmonary flow.
Is right‑heart catheterisation painful?
The procedure is performed under local anesthesia with mild sedation. Most patients feel only a brief pressure sensation; serious complications are rare (<1%).
What are the latest treatment options for early‑stage PAH?
Combination therapy using an endothelin‑receptor antagonist (e.g., ambrisentan) plus a phosphodiesterase‑5 inhibitor (e.g., tadalafil) is now first‑line for WHO functional classII. Oral prostacyclin receptor agonists are added if the combo isn’t enough.
