Opioid Side Effects: What You Need to Know Before Taking Them
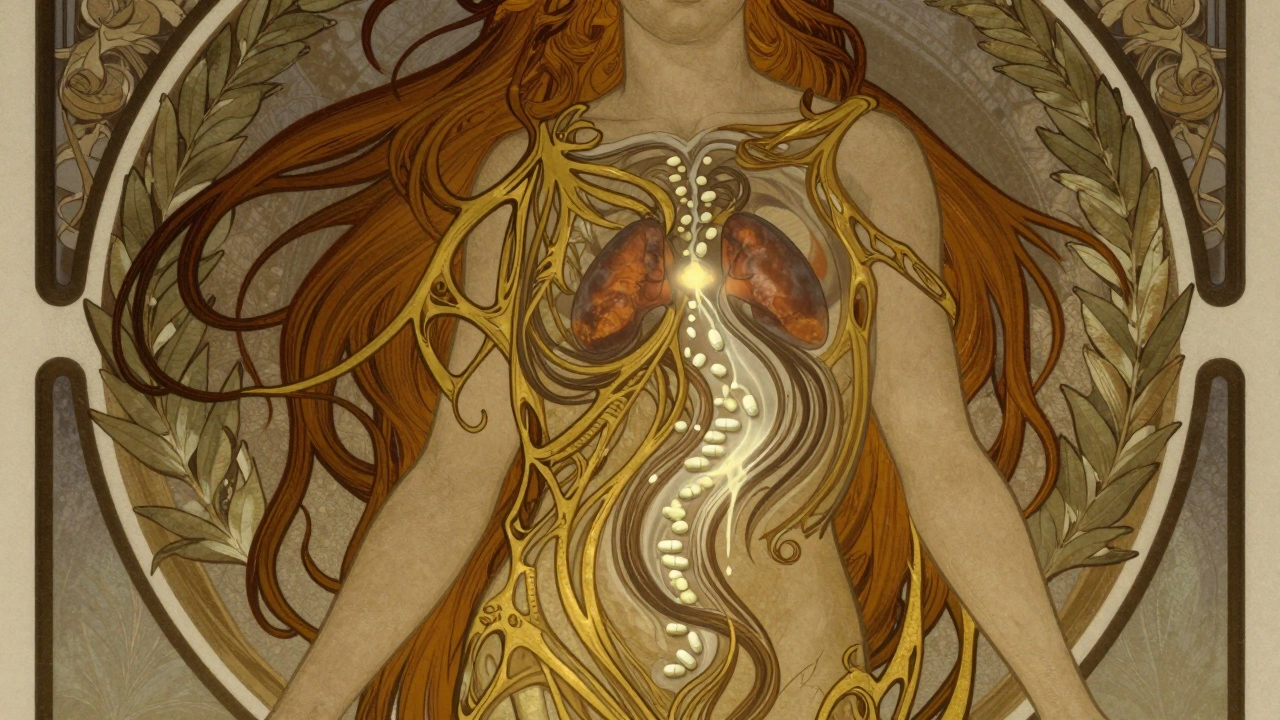
When you take opioids, a class of powerful pain-relieving drugs that include oxycodone, hydrocodone, morphine, and fentanyl. Also known as narcotics, they work by binding to receptors in your brain and spinal cord to block pain signals. But they don’t just turn off pain—they also slow your breathing, change how your gut moves, and can rewire your brain over time. That’s why opioid side effects aren’t just inconvenient—they can be dangerous.
One of the most serious risks is respiratory depression, when breathing slows so much that oxygen levels drop dangerously low. This isn’t rare—it’s the leading cause of death in opioid overdoses. Even people taking prescribed doses can experience this, especially if they mix opioids with alcohol, benzodiazepines, or sleep aids. Another common but often ignored effect is constipation, a side effect so widespread that up to 90% of long-term users struggle with it. Unlike nausea or drowsiness, constipation doesn’t fade with time. It just gets worse, and many people don’t tell their doctors because they think it’s normal.
Then there’s opioid dependence, when your body adapts to the drug and needs it to feel normal. This isn’t addiction—it’s a physical change. You might not crave the drug, but if you skip a dose, you start sweating, shaking, and feeling sick. That’s opioid withdrawal, a set of intense symptoms that can include muscle aches, diarrhea, vomiting, and anxiety. It’s not usually deadly, but it’s brutal enough to make people go back on the drug just to feel okay again.
These side effects don’t happen to everyone at the same time, but they’re predictable. The longer you take opioids, the higher the risk. The higher the dose, the worse they get. And if you’ve had a history of substance use, mental health issues, or sleep apnea, your chances go up even more. That’s why slow up-titration schedules—like the ones used for GLP-1 agonists and beta-blockers—are sometimes recommended even for opioids, to help your body adjust without overwhelming it.
What’s often missing from the conversation is that these side effects aren’t always unavoidable. There are ways to manage them—laxatives for constipation, naloxone on hand for emergencies, non-opioid pain treatments like physical therapy or anti-inflammatories. Some people find relief with cognitive behavioral therapy, which helps rewire how the brain processes pain signals without drugs. And if you’re on opioids long-term, knowing how to recognize early signs of dependence or respiratory issues can literally save your life.
You’ll find real stories here—how people caught the warning signs before it was too late, what worked when standard advice failed, and which alternatives actually helped them get off opioids without losing pain control. These aren’t theory-based guides. They’re from people who lived it. If you’re on opioids, or know someone who is, this collection gives you the facts you won’t get from a pharmacy label.
Opioids and Adrenal Insufficiency: A Rare but Life-Threatening Side Effect You Need to Know
Caspian Mortensen Dec, 1 2025 13Opioid-induced adrenal insufficiency is a rare but life-threatening side effect of long-term opioid use. It suppresses the body's stress response and can lead to adrenal crisis if undiagnosed. Learn who's at risk and what to do.
More Detail