Antihistamine Interactions with Other Sedating Medications: What You Need to Know

Oct, 28 2025
Anticholinergic Burden Calculator
Add Your Medications
How It Works
The Anticholinergic Cognitive Burden (ACB) scale rates medications from 0 to 3 based on their potential to cause cognitive impairment.
The higher your total score, the greater your risk of dangerous interactions with sedating medications like:
- Benzodiazepines (Xanax, Valium)
- Opioids (Oxycodone, Codeine)
- Alcohol
- Other sedating medications
A total score of 3 or higher indicates high risk for cognitive decline and dangerous interactions.
Your Medications
Combining antihistamines with other sedating medications can be more dangerous than most people realize. You might think taking Benadryl for allergies before bed is harmless, especially if you’re also using a sleep aid or anxiety medication. But when these drugs mix, they don’t just add up-they multiply. The result? Extreme drowsiness, confusion, slowed breathing, or even hospitalization. This isn’t a rare accident. It’s a predictable risk that happens every day, often because people don’t know what they’re mixing.
Why First-Generation Antihistamines Are the Real Problem
Not all antihistamines are the same. There are two main types: first-generation and second-generation. The first-generation ones-like diphenhydramine (Benadryl), hydroxyzine, and promethazine-are the ones you need to worry about. They were developed in the 1940s and were designed to cross into the brain. That’s how they stop sneezing and itching. But it’s also why they make you sleepy, dizzy, and foggy-headed. These drugs don’t just block histamine. They also block acetylcholine, a brain chemical that keeps you alert. This is called anticholinergic activity. On the Anticholinergic Cognitive Burden (ACB) scale, diphenhydramine scores a 3-the highest level. That means even one dose can impair memory and coordination, especially in older adults. When you add another sedating drug on top, like a benzodiazepine or opioid, the effect isn’t just stronger-it’s unpredictable. Second-generation antihistamines like loratadine (Claritin), cetirizine (Zyrtec), and fexofenadine (Allegra) were made to avoid this. They’re designed to stay out of the brain. They work just as well for allergies but don’t cause the same level of drowsiness. Studies show 97% of people taking loratadine report no drowsiness, compared to 68% on diphenhydramine. That’s not a small difference. It’s the difference between driving safely and being impaired.Which Medications Are Most Dangerous to Mix?
The biggest risks come from combining first-generation antihistamines with other central nervous system (CNS) depressants. Here are the most common and dangerous combinations:- Benzodiazepines: Drugs like lorazepam (Ativan), alprazolam (Xanax), and diazepam (Valium) are prescribed for anxiety and sleep. When mixed with diphenhydramine, sedation increases by up to 42%, according to clinical studies. One Reddit user described a near-fatal experience after taking 50mg of Benadryl with 1mg of Xanax-respiratory depression, blacking out, and a trip to the ER.
- Opioids: Painkillers like oxycodone, hydrocodone, and codeine already carry a risk of slowed breathing. Add diphenhydramine, and that risk jumps from 1.5% to 8.7%. The CDC reports that 41% of patients taking both experienced severe dizziness requiring medical attention.
- Alcohol: Even one drink with 25mg of diphenhydramine can cause complete blackouts. BuzzRx documented over 1,200 user reports of hospital visits after mixing alcohol and Benadryl. It’s not just about being drunk-it’s about your body losing the ability to control breathing.
- Sleep aids: Many over-the-counter sleep medications contain diphenhydramine or doxylamine. Taking them with another sedating drug-like a muscle relaxer or antidepressant-is like pouring gasoline on a fire.
- Anticholinergic drugs: Medications like oxybutynin (for overactive bladder) or tricyclic antidepressants add to the anticholinergic load. A 2021 JAMA study found that combining these with first-gen antihistamines increased delirium risk by 54% in older adults.
Why Older Adults Are at the Highest Risk
As we age, our bodies process drugs differently. The liver and kidneys slow down. Clearance of diphenhydramine drops by 50-70% in people over 65. That means the drug stays in the system longer, building up over time. Even small doses become dangerous. The American Geriatrics Society has listed first-generation antihistamines on its Beers Criteria since 2015-and updated it again in 2024 to include hydroxyzine. This isn’t a suggestion. It’s a warning: avoid these drugs in older adults. Why? Because they’re linked to falls, confusion, memory loss, and even dementia. A 2015 study found that long-term use of anticholinergic drugs, including diphenhydramine, was associated with a 54% increased risk of dementia. Many seniors take multiple medications. The average Medicare beneficiary takes nearly 8 prescriptions. When you stack drugs with sedative or anticholinergic effects, the risk compounds. A doctor might prescribe an antihistamine for allergies, a benzodiazepine for anxiety, and an anticholinergic for bladder control. None seem dangerous alone. Together? They’re a storm waiting to happen.
What About Second-Generation Antihistamines?
Here’s the good news: second-generation antihistamines are far safer. Drugs like cetirizine, loratadine, fexofenadine, and the newer bilastine have ACB scores of 0 or 1. They don’t cross the blood-brain barrier significantly. Studies show they don’t increase sedation when taken with benzodiazepines or opioids. For example, a 2023 study in the Journal of Clinical Psychopharmacology found that bilastine-even at double the normal dose-had no interaction with lorazepam. That’s a breakthrough. It means future antihistamines may eliminate this risk entirely. But don’t assume “nondrowsy” means “no risk.” Cetirizine still has a low ACB score of 1, and in people with liver or kidney problems, it can build up. It’s safer, but not risk-free. Still, for most people, especially those on other medications, switching to a second-generation antihistamine is the single best step you can take.How to Stay Safe: Practical Steps
You don’t need to be a pharmacist to protect yourself. Here’s what to do:- Check every medication label. Look for diphenhydramine, doxylamine, or promethazine. These are hidden in sleep aids, cold medicines, and even some stomach remedies.
- Use the ACB scale. The University of Washington has a free online calculator. Add up the scores of all your meds. If your total is 3 or higher, talk to your doctor. High anticholinergic burden is linked to cognitive decline.
- Ask your pharmacist. Pharmacists are trained to spot dangerous combinations. Bring a list of everything you take-even supplements and OTC drugs.
- Switch to second-generation antihistamines. If you’re taking Benadryl for allergies, ask for Claritin, Zyrtec, or Allegra instead. They work just as well without the danger.
- Don’t use antihistamines as sleep aids. They’re not designed for long-term sleep. They disrupt deep sleep cycles and increase fall risk. If you have trouble sleeping, talk to your doctor about safer options.
What’s Changing in the Market
Awareness is growing. Since 2018, sales of first-generation antihistamines have dropped 12.7% each year. Second-generation drugs now make up 83% of the $2.4 billion U.S. OTC antihistamine market. The FDA now requires bold warnings on diphenhydramine packaging: “May cause severe drowsiness when combined with alcohol, opioids, or sleep medications.” Health systems like Kaiser Permanente have added automated alerts in their electronic records. Since 2020, they’ve cut antihistamine-related adverse events by 34%. That’s not just technology-it’s saved lives. The future is moving toward precision medicine. A 2024 study in Nature Medicine found that people with a CYP2D6 gene variant (poor metabolizers) process diphenhydramine 3.2 times slower. That means they’re at even higher risk. In the coming years, genetic testing may help doctors choose safer antihistamines before a single pill is taken.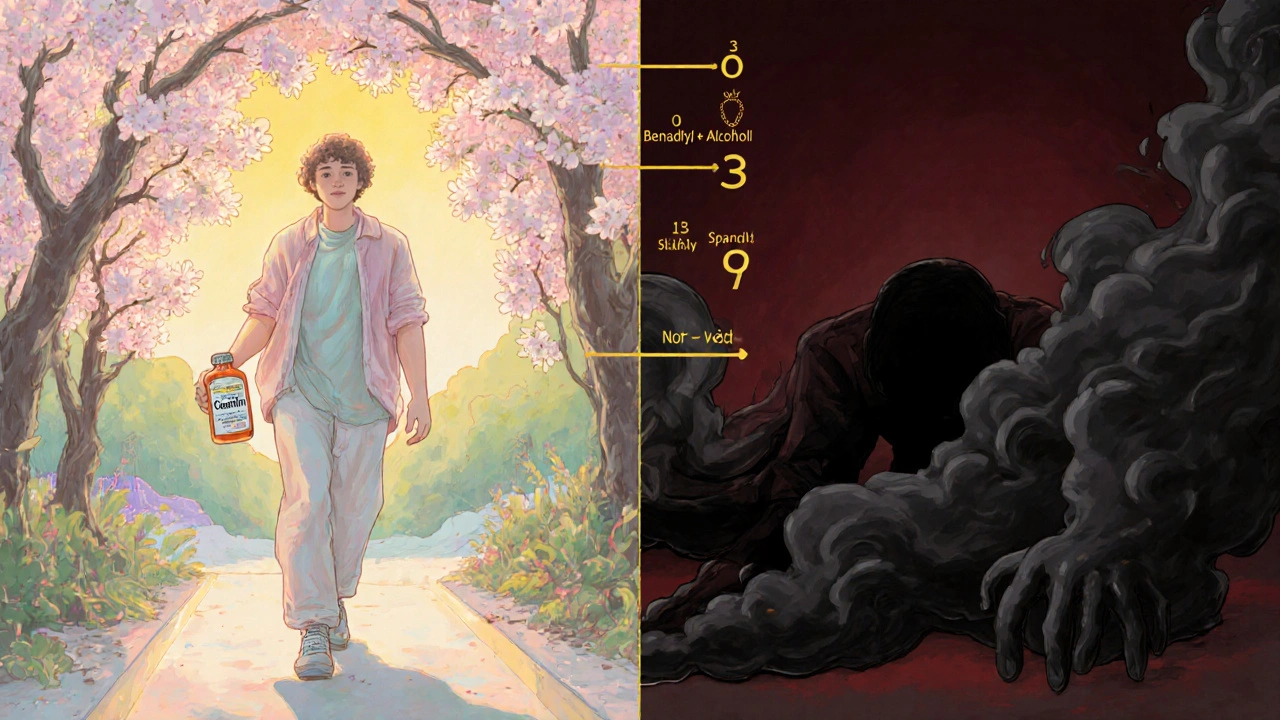
When Is It Okay to Use First-Generation Antihistamines?
There are exceptions. For short-term, acute use-like treating motion sickness with dimenhydrinate (Dramamine) or managing severe allergic reactions-they’re still useful. In palliative care, doctors sometimes use diphenhydramine with benzodiazepines to calm terminal agitation. But these are tightly controlled, monitored situations. For everyday allergies, itching, or sleep? There’s no justification anymore. Safer, equally effective alternatives exist. Continuing to use first-generation antihistamines in these cases isn’t tradition-it’s unnecessary risk.What to Do If You’ve Already Mixed Them
If you’ve taken a first-generation antihistamine with another sedating drug and feel unusually drowsy, confused, or have trouble breathing-don’t wait. Call 911 or go to the nearest ER. These reactions can escalate quickly. If you’re unsure whether your meds are interacting, use the Institute for Safe Medication Practices’ free Antihistamine Interaction Checker. It’s simple, reliable, and updated with the latest data.Final Thought: Your Medications Are a Team
Medicines don’t work in isolation. They talk to each other. Sometimes, they help. Sometimes, they fight. And sometimes, they team up to hurt you. Antihistamines are no exception. The key isn’t avoiding all meds-it’s choosing the right ones and knowing what they’re doing together. If you’re on more than three medications, especially if you’re over 65, ask your doctor: Is this antihistamine necessary? Is there a safer version? That one question could prevent a hospital stay-or worse.Can I take Benadryl with Xanax?
No. Combining diphenhydramine (Benadryl) with alprazolam (Xanax) significantly increases sedation and can lead to dangerous respiratory depression. Multiple user reports and clinical studies show this combination has caused hospitalizations. Use a second-generation antihistamine like loratadine instead if you need allergy relief while taking anxiety medication.
Are all antihistamines equally sedating?
No. First-generation antihistamines like diphenhydramine and hydroxyzine cross into the brain and cause strong drowsiness. Second-generation antihistamines like loratadine, cetirizine, and fexofenadine are designed to stay out of the brain and rarely cause sedation. Check the label-only first-generation ones contain diphenhydramine or doxylamine.
Is Zyrtec safe with other medications?
Cetirizine (Zyrtec) is a second-generation antihistamine and generally safer than Benadryl. However, it still has a low anticholinergic burden (ACB score of 1) and can interact with strong CNS depressants like opioids or alcohol, especially in older adults or those with kidney issues. It’s much safer than first-gen options, but not risk-free.
Why do doctors still prescribe Benadryl?
Benadryl is cheap, widely available, and effective for acute allergic reactions. But for routine allergy or sleep use, it’s outdated. Many doctors prescribe it out of habit or because patients ask for it. The American College of Allergy, Asthma & Immunology now recommends second-generation antihistamines as first-line treatment. Ask your doctor if there’s a better option.
Can antihistamines cause dementia?
Long-term use of high-anticholinergic drugs-including diphenhydramine-has been linked to a 54% increased risk of dementia, according to a 2015 study. This doesn’t mean one dose causes it, but regular use over years adds up. The American Geriatrics Society advises avoiding these drugs in older adults for this exact reason.
What should I do if I’m taking multiple sedating drugs?
Schedule a medication review with your doctor or pharmacist. Bring a full list of everything you take, including OTC drugs and supplements. Ask specifically about anticholinergic burden and CNS depressant interactions. You may be able to replace one or more drugs with safer alternatives. Don’t stop anything on your own-work with a professional.
