GERD and Bisphosphonates: How to Prevent Esophageal Irritation
Dec, 10 2025
Bisphosphonate Safety Calculator
This calculator helps you assess your risk of esophageal irritation when taking bisphosphonate medications like Fosamax or Actonel. Follow the guidelines in the article to minimize your risk.
Your results will appear here after clicking the button above.
If you’re taking a bisphosphonate like alendronate (Fosamax) or risedronate (Actonel) for osteoporosis and you also have GERD, you’re at higher risk for serious esophageal irritation. This isn’t just a mild upset stomach-it’s a real chance of developing esophagitis, ulcers, or even bleeding in the esophagus. The good news? Most of these problems are preventable if you know how to take these medications correctly.
Why Bisphosphonates Hurt Your Esophagus
Bisphosphonates are powerful drugs. They work by slowing down bone loss, cutting fracture risk by 40% to 70% in people with osteoporosis. But they’re also highly acidic. When you swallow a pill, it doesn’t dissolve like a regular tablet. Instead, it sits in your esophagus, and if it’s not washed down quickly or if stomach acid backs up, it starts to burn the lining. The science behind it is simple: when the pH in your esophagus drops below 2.0, alendronate turns from a safe salt form into a free acid. That acid doesn’t just irritate-it can cause chemical burns. Studies show that 0.7% of people taking alendronate develop esophagitis, compared to 0.4% on placebo. That might sound low, but for someone with GERD, the risk jumps significantly. In fact, people with existing reflux are nearly five times more likely to suffer damage.GERD Makes It Worse
GERD isn’t just heartburn. It means your lower esophageal sphincter isn’t closing right, letting stomach acid flow back up. When you take a bisphosphonate with GERD, two things happen: the pill sits longer in your esophagus because of slow movement, and acid from your stomach coats it. This double hit increases the chance of injury. A 2023 case study tracked a 72-year-old woman who took her alendronate pill and immediately lay down to rest. Within hours, she developed severe chest pain. An endoscopy showed deep, patchy ulcers in her esophagus. She needed hospitalization. This isn’t rare. In one study, 10.7% of bisphosphonate users reported esophageal symptoms-dysphagia, burning, regurgitation. About 1 in 10 people. And here’s the twist: some studies found that people on alendronate actually had less reflux esophagitis than placebo. Why? Because the drug itself causes a different kind of damage-localized chemical burns-not the widespread inflammation from acid reflux. But if you already have reflux, you’re more likely to get both.The Rules for Taking Bisphosphonates Safely
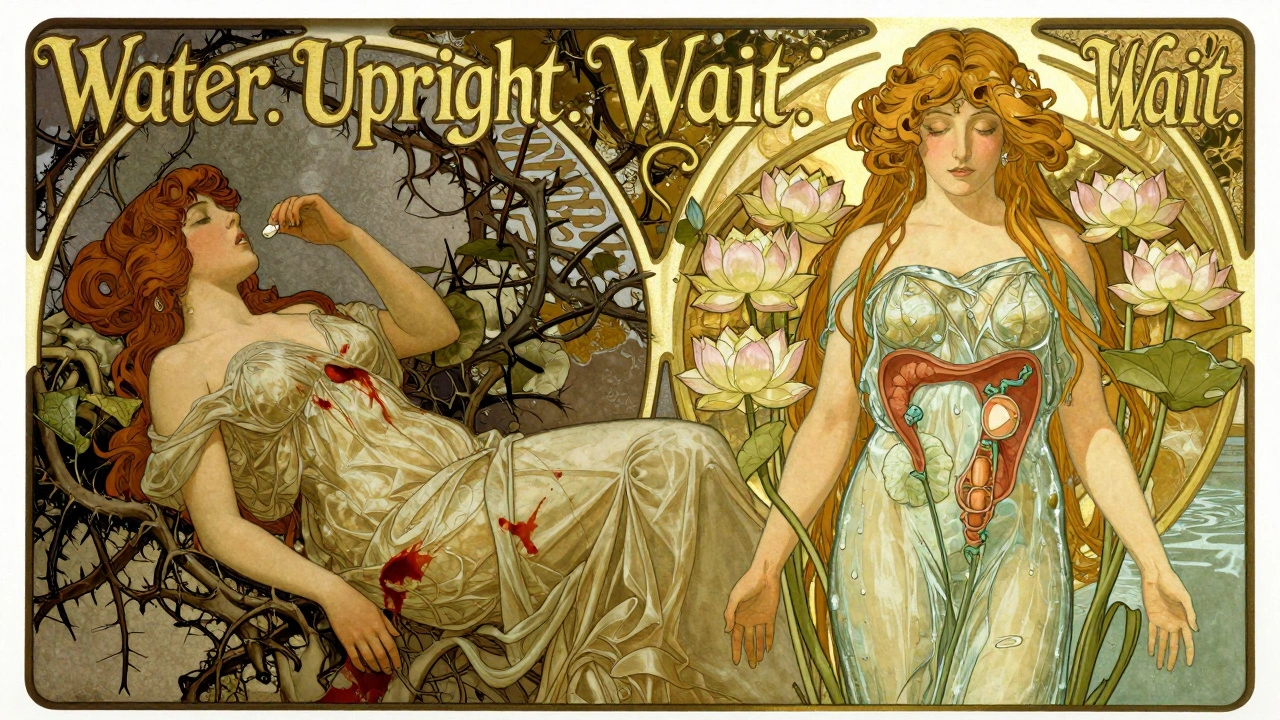
The FDA and major medical groups agree: if you take an oral bisphosphonate, you must follow these steps exactly.- Take it first thing in the morning, on an empty stomach. No coffee, no juice, no food.
- Use a full glass of plain water-6 to 8 ounces. Don’t use mineral water, sparkling water, or tea. Minerals in those drinks can bind to the drug and make it less effective-or worse, increase irritation.
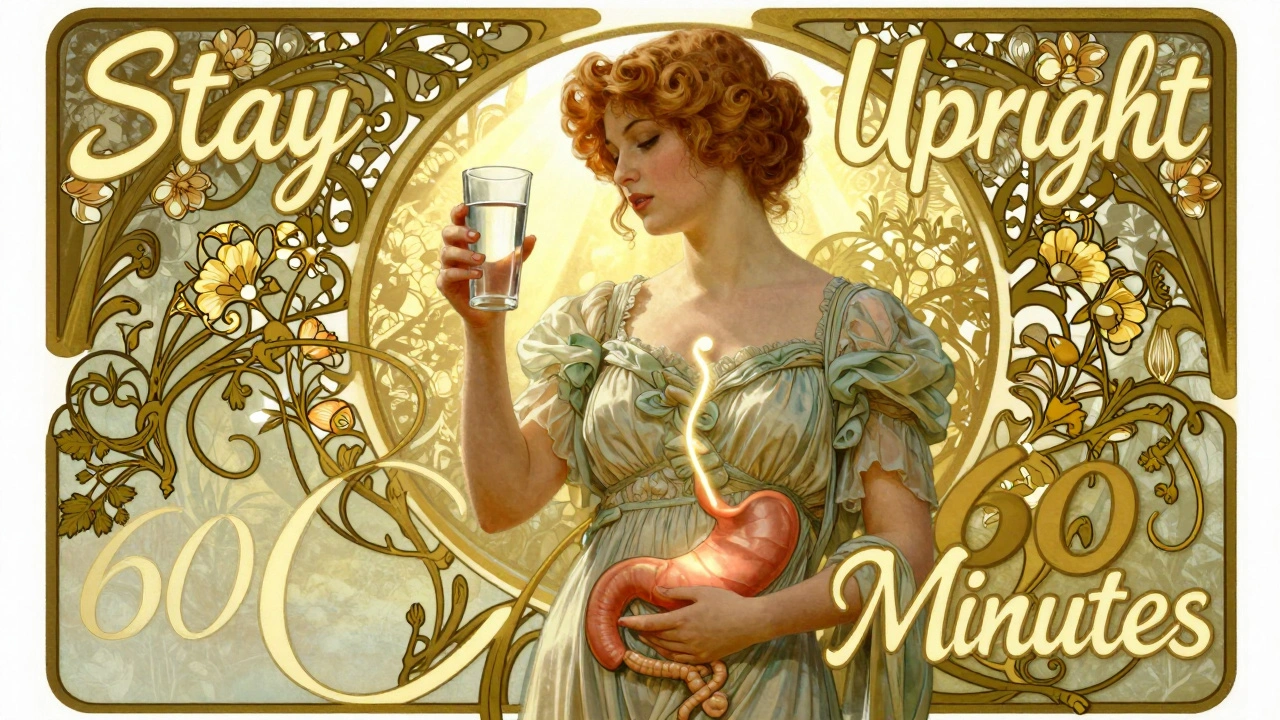
- Stay upright-sitting or standing-for at least 60 minutes after taking it. No lying down. No reclining. No bending over to pick something up. This gives the pill time to pass through your esophagus and into your stomach.
- Wait 60 minutes before eating, drinking, or taking any other medicine. Even a sip of water too soon can trap the pill in your esophagus.
- Don’t take it at night. Even if you’re tired, lying down after a pill is a recipe for trouble.
What If You Already Have GERD?
If you’ve been diagnosed with GERD, you’re not automatically ruled out from bisphosphonates-but you need to be extra careful. Talk to your doctor before starting. Ask:- Have you had an endoscopy recently to check for esophageal damage?
- Are you on a proton pump inhibitor (PPI) like omeprazole or esomeprazole? If not, you might need one.
- Have you ever had trouble swallowing or had an esophageal stricture?
Alternatives to Oral Bisphosphonates
Not everyone needs to take a pill. Here’s how the options stack up:| Treatment | Route | Esophageal Risk | Cost (Monthly) | Fracture Risk Reduction |
|---|---|---|---|---|
| Alendronate (Fosamax) | Oral, weekly | High | $0.50-$1.00 | 44-50% |
| Risedronate (Actonel) | Oral, weekly or monthly | High | $1-$3 | 40-70% |
| Denosumab (Prolia) | Subcutaneous injection | None | $1,500+ | 68% |
| Zoledronic acid (Reclast) | IV infusion | None | $1,200-$1,500/year | 70% |
| Romosozumab (Evenity) | Subcutaneous injection | None | $5,000/month | 73% |

What to Do If You Feel Burning After Taking the Pill
If you take your bisphosphonate correctly and still get:- Chest pain that doesn’t go away
- Difficulty swallowing
- Feeling like food is stuck
- Vomiting blood or black, tarry stools
Real Stories, Real Results
On Reddit’s osteoporosis community, one user wrote: “I had heartburn every time I took Fosamax. I thought it was just my GERD acting up. Then I read the instructions again-turns out I was taking it with half a glass of water and lying down 10 minutes later. I changed everything: full glass, upright for an hour, no food. The burning vanished in two weeks.” Another user, 78, switched to zoledronic acid after three episodes of esophagitis. “I hated shots,” she said. “But I hated the pain more. Now I’m pain-free and my bones are stronger.” These aren’t outliers. They’re proof that small changes make a big difference.The Bottom Line
Bisphosphonates save lives by preventing fractures. But they can hurt your esophagus-if you don’t take them right. If you have GERD, you need to be smarter about it. Follow the rules. Ask for alternatives. Don’t assume the pill will be fine just because your doctor prescribed it. The goal isn’t to avoid treatment. It’s to get the benefit without the damage. And that’s possible-if you know how.Can I take bisphosphonates if I have GERD?
Yes, but only if you follow strict dosing rules: take it with a full glass of plain water, stay upright for 60 minutes, and never lie down afterward. If you still get symptoms, talk to your doctor about switching to an injectable like denosumab or zoledronic acid, which don’t touch your esophagus.
How long should I wait after taking a bisphosphonate before eating?
Wait at least 60 minutes after taking the pill before eating, drinking anything other than plain water, or taking other medications. Even a small snack or sip of coffee too soon can trap the drug in your esophagus and cause irritation.
Is it safe to take a bisphosphonate with a proton pump inhibitor (PPI)?
Yes, many doctors prescribe PPIs like omeprazole alongside bisphosphonates for patients with GERD. PPIs reduce stomach acid, which helps lower the risk of esophageal damage. But they don’t replace the need for proper dosing-staying upright and using enough water is still essential.
What are the signs of esophageal damage from bisphosphonates?
Watch for persistent chest pain, difficulty swallowing, feeling like food is stuck, or vomiting blood. These aren’t normal side effects-they signal possible ulcers or bleeding. Stop the medication and contact your doctor right away. An endoscopy is needed to confirm damage.
Are there safer alternatives to oral bisphosphonates?
Yes. Denosumab (Prolia) is a monthly injection that doesn’t affect the esophagus. Zoledronic acid (Reclast) is a once-a-year IV infusion. Both are effective at reducing fractures and avoid the risk of chemical esophagitis. The trade-off is cost and the need for injections or infusions.
Can bisphosphonates cause esophageal cancer?
Current evidence doesn’t support a clear link. Some early studies suggested a possible risk, but larger, more recent research-including the NIH’s ongoing Bisphosphonate Safety Study-shows no significant increase in esophageal cancer risk after five years of use. The FDA still monitors this, but the main concern remains acute irritation and ulcers, not cancer.
