Fentanyl Patch Side Effects: Overdose and Withdrawal Risks Explained

Jan, 10 2026
Fentanyl Patch Safety Checklist
Use this checklist to ensure you're following critical safety guidelines for fentanyl patch use. Check each item that applies to your current situation.
Avoid using patches on damaged skin or areas where clothing rubs.
No hot tubs, saunas, heating pads, electric blankets, or sunbathing while wearing a patch.
A single used patch contains enough fentanyl to kill a child.
Fold sticky side over itself and dispose of in trash, not toilet.
Never share fentanyl patches with anyone.
Naloxone can reverse a fentanyl overdose if administered quickly.
Never change patch strength or frequency without consulting your doctor.
Avoid alcohol, benzodiazepines, sleep aids, or other depressants while using patches.
Using a fentanyl patch might seem like a simple way to manage chronic pain, but the risks are serious - and often misunderstood. These patches deliver a powerful opioid directly through the skin, 24 hours a day, for three days straight. That steady flow is great for pain control, but it also means there’s no off switch. If something goes wrong - if you get too hot, if you take it wrong, or if you stop suddenly - the consequences can be deadly.
How Fentanyl Patches Work - and Why That’s Dangerous
Fentanyl patches are designed for people with severe, long-term pain who’ve already been on opioids and need constant relief. They’re not for occasional pain, surgery recovery, or anyone who’s never taken opioids before. The patch contains a gel-like reservoir of fentanyl, a synthetic opioid 50 to 100 times stronger than morphine. It slowly leaks through your skin into your bloodstream, reaching full strength after 12 to 24 hours. Once it’s in, it stays in - for 72 hours. That’s the problem. Unlike pills you can skip or cut back on, the patch keeps working even if you feel fine. If your body heats up - from a fever, a hot shower, a heating pad, or even lying in the sun - the patch releases even more fentanyl. This can push your system into overdose territory without you realizing it. The FDA has documented cases where people died after using a heating pad with their patch on.Overdose: What It Looks Like and What to Do
An overdose from a fentanyl patch doesn’t always come with screaming or panic. Often, it’s quiet. You might notice someone becoming unusually sleepy, hard to wake up, or breathing very slowly - less than 8 breaths a minute. Their skin turns cold and clammy. Their lips or fingernails might look blue. Their pupils shrink to pinpoints. They might go limp, like a ragdoll. If you see any of these signs, act immediately. Remove the patch. Call emergency services right away. Don’t wait. Don’t try to wake them with coffee or cold water. Time matters. Fentanyl overdoses can kill in minutes. Doctors now routinely prescribe naloxone (Narcan) with fentanyl patches. It’s a nasal spray or injection that can reverse the overdose. Keep it in your medicine cabinet, not the back of a drawer. Teach family members how to use it. The FDA now recommends naloxone be offered to everyone prescribed any long-acting opioid, not just those with a history of misuse.Withdrawal: The Hidden Danger of Stopping Too Fast
Many people assume that if they stop taking a painkiller, they’ll just feel better. With fentanyl patches, that’s a myth. If you’ve been using the patch for more than a few weeks, your body adapts. It changes how your brain and nerves work to handle the constant opioid presence. Stop suddenly, and your body goes into chaos. Withdrawal hits within 8 to 24 hours after your last patch. It peaks at 2 to 3 days and can last over a week. Symptoms aren’t just uncomfortable - they’re brutal. You’ll feel restless, anxious, and irritable. Your muscles will ache. You’ll sweat like you’re running a marathon, even when you’re sitting still. Your nose will run. You’ll yawn nonstop. You’ll get stomach cramps, vomiting, and diarrhea. Your heart races. Your blood pressure spikes. Sleep becomes impossible. The worst part? Withdrawal can make you want to use fentanyl again - just to feel normal. That’s how relapses happen. And here’s the deadly twist: after even a short break, your tolerance drops. Your body forgets how to handle the drug. If you take the same dose you used before, you can overdose - even if you think you’re still used to it. Johns Hopkins found that 37% of fatal fentanyl overdoses happened in people who had recently stopped using.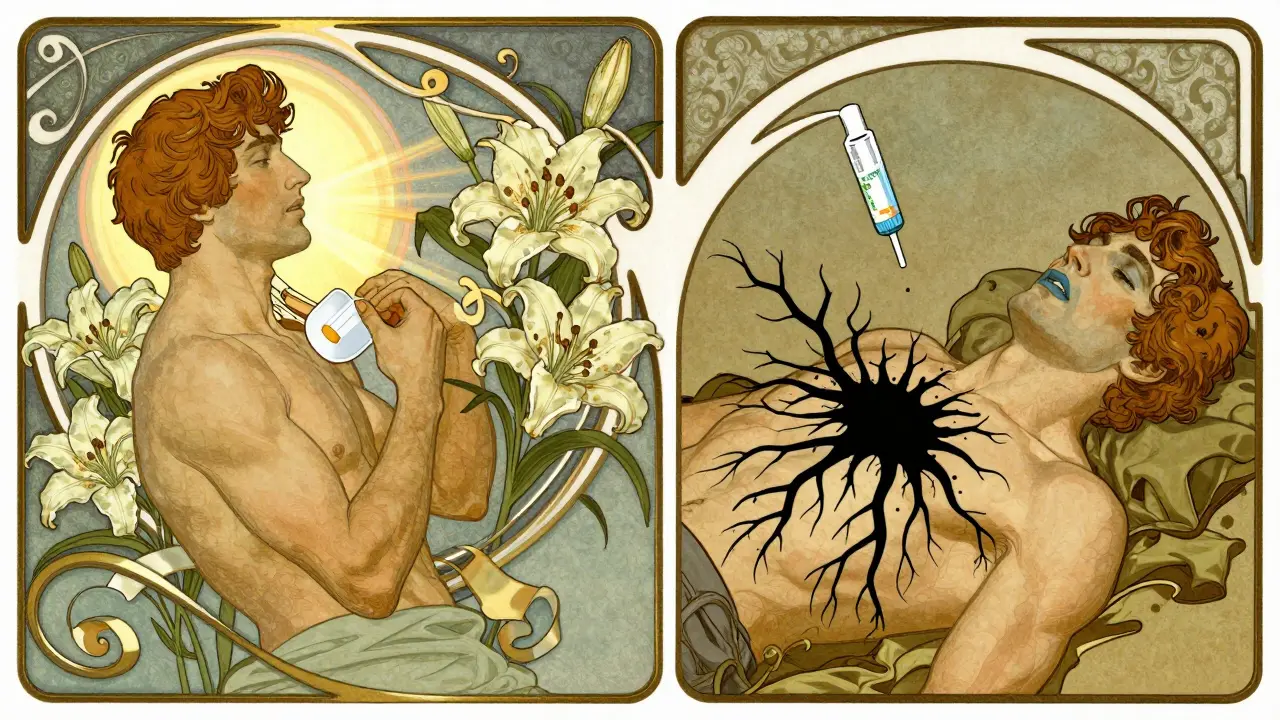
How to Stop Safely - No Guesswork
Never stop a fentanyl patch on your own. Never cut the dose in half. Never skip a day. The only safe way is a slow, doctor-supervised taper. The European Medicines Agency says reducing the dose by 10% to 25% every 1 to 3 weeks is typical. For someone on a high dose, that might take months. Your doctor will adjust based on how you feel - not on a calendar. During the taper, you might still feel some withdrawal symptoms. That’s normal. But if they become unbearable, your doctor can add medications to help - like clonidine for anxiety and high blood pressure, or anti-nausea drugs. Some patients benefit from short-term use of non-opioid pain relievers or antidepressants to manage nerve pain. The key is communication. Tell your doctor if you’re feeling worse, not better. If you’re tempted to go back to your old dose, talk to them before you do it.What You Must Do Every Day
Safety isn’t just about stopping or overdosing. It’s about daily habits.- Apply patches only to clean, dry, intact skin. No cuts, rashes, or burns. Avoid areas where your skin rubs against clothes.
- Avoid heat. No hot tubs, saunas, heating pads, electric blankets, or sunbathing while wearing a patch.
- Keep patches away from children and pets. A single used patch still contains enough fentanyl to kill a child. The FDA reported 32 pediatric deaths between 1997 and 2012 from accidental exposure.
- Dispose of used patches properly. Fold the sticky side over itself, then throw it in the trash - not the toilet. Some pharmacies offer take-back programs.
- Never share your patches. Even if someone else has chronic pain, they’re not tolerant to fentanyl. It could kill them.
- Tell every doctor and dentist you see. You might need to pause your patch before surgery or dental work. Fentanyl interacts with many other drugs, including benzodiazepines, sleep aids, and alcohol.
Why These Patches Are Being Used Less
Prescriptions for fentanyl patches dropped 42% between 2016 and 2022. Why? Because doctors now know the risks better. The CDC says fentanyl patches should only be used if you’re already opioid-tolerant - meaning you’ve been taking at least 60 mg of morphine daily for a week or more. Most doctors now try non-opioid options first: physical therapy, nerve blocks, anti-inflammatory meds, or even cognitive behavioral therapy for pain. In 2023, 78% of physicians said they only consider fentanyl patches after all other options fail. That’s up from 52% in 2016. The FDA’s mandatory training for prescribers has helped. But the real change? Patients are asking more questions. They’re demanding safer alternatives.
What’s Next? Safer Patches on the Horizon
Researchers are working on new versions of fentanyl patches that reduce overdose risk. Two clinical trials are testing patches with built-in limits - like a chemical barrier that stops too much fentanyl from leaking if the skin heats up. Others are adding sensors to alert users if the patch is removed or tampered with. But until those are available, the safest approach is simple: use the patch exactly as prescribed, never mix it with heat or other depressants, keep it out of reach of others, and never stop it cold turkey.Frequently Asked Questions
Can I cut a fentanyl patch in half to lower my dose?
No. Cutting a fentanyl patch destroys its controlled-release design. It can cause a dangerous surge of fentanyl into your bloodstream, leading to overdose. Always change the patch strength using a new prescription - never cut or alter the patch.
Is it safe to use a fentanyl patch if I drink alcohol?
No. Alcohol slows your breathing and increases sedation. Combined with fentanyl, this dramatically raises your risk of respiratory failure and death. Even one drink can be dangerous. Avoid alcohol completely while using the patch.
How long does fentanyl stay in my system after I stop the patch?
Fentanyl can remain detectable in your blood for up to 3 days after removing the patch, and in urine for up to 72 hours. But its effects on your brain and body - especially your tolerance - last much longer. Withdrawal symptoms can linger for weeks, and your sensitivity to opioids stays lowered for months. Don’t assume you’re "clean" just because the patch is off.
Can I use a fentanyl patch for sudden pain, like a back spasm?
No. Fentanyl patches are not meant for sudden or short-term pain. They take 12 to 24 hours to reach full effect and last for 72 hours. Using them for acute pain can lead to dangerous buildup of the drug in your system. Use fast-acting pain relievers like ibuprofen or short-acting opioids (if prescribed) instead.
What should I do if I accidentally leave a patch on too long?
Remove it immediately. If you feel dizzy, sleepy, or have trouble breathing, call emergency services. Even if you feel fine, contact your doctor. You may need to skip your next patch or reduce your dose to avoid overdose. Never try to "catch up" by applying a new patch sooner.
Are there safer alternatives to fentanyl patches for chronic pain?
Yes. Many patients find relief with non-opioid treatments like physical therapy, nerve blocks, acupuncture, or medications like gabapentin or duloxetine. For those who still need opioids, shorter-acting options like extended-release oxycodone or morphine may be safer - especially if you’re not already opioid-tolerant. Always discuss alternatives with your doctor before starting fentanyl.
What to Do Next
If you’re currently using a fentanyl patch:- Check your prescription label. Does it say you’re opioid-tolerant? If not, ask your doctor why you’re on it.
- Find out if you have naloxone. If not, ask for a prescription.
- Review your patch use with your doctor. Are you still getting pain relief? Are you feeling more tired than usual? Are you avoiding heat?
- Start a pain diary. Write down your pain levels, side effects, and any changes in how you feel. Bring it to your next appointment.
- Don’t quit on your own.
- Ask your doctor for a taper plan - not just a number, but a timeline and backup options if symptoms flare.
- Ask if a pain specialist or addiction medicine doctor can help you through the process.
