How to Communicate Generic Substitution to Pediatric and Senior Patients

Jan, 7 2026
When a pharmacist hands you a pill that looks completely different from what you’ve been taking for years, it’s natural to feel uneasy. For parents of young children or seniors managing multiple prescriptions, this moment can spark fear, confusion, or even refusal to take the medicine. Generic substitution is common - generic drugs make up 90% of all prescriptions filled in the U.S. - but explaining it well isn’t automatic. Many patients think a different-looking pill means a weaker drug. That’s not true. But if you don’t explain it right, they’ll believe it anyway.
Why Generic Substitution Feels Risky for Kids and Seniors
For children, the issue isn’t just about active ingredients. It’s about taste, texture, and how the medicine is delivered. Brand-name pediatric versions often come as sweetened liquids, chewable tablets, or easy-to-swallow capsules. Generic versions? Many are tablets or bitter suspensions. A 2020 study found that only 32% of generic pediatric medications come in child-friendly forms, compared to 68% of brand-name ones. One parent on Reddit shared that her 2-year-old refused the generic amoxicillin because it tasted like “burnt plastic.” She had to switch back, even though it cost $40 more per prescription. That’s not just a cost issue - it’s an adherence issue. If the child won’t take it, the infection doesn’t go away. For seniors, the problem is complexity. The average older adult takes 4.8 prescription drugs. When one pill changes shape, color, or size - even if it’s the same active ingredient - they might think it’s a different medication. A 78-year-old man in Florida stopped taking his blood pressure pill after it changed three times in six months. He thought he was being given the wrong drug. He didn’t know it was still the same medicine, just a different generic version. That’s not rare. In fact, 52% of seniors report confusion when their medications change appearance over time.The Nocebo Effect: When Expectations Make You Sick
Here’s the hidden danger: the nocebo effect. That’s when people feel side effects because they expect them - not because the drug is doing anything different. A 2021 study in Frontiers in Pharmacology found that 58% of seniors reported new side effects after switching to a generic - even though the active ingredient hadn’t changed. The same study showed younger adults reported side effects at only 42%. Why? Because seniors were told, “This is cheaper now,” or “It’s the same, but different-looking.” That sets the mind up to notice anything unusual - a headache, a stomach ache - and blame the pill. Parents feel this too. A 2020 Pediatrics survey found that 62% of parents were hesitant about generics, worried their child’s condition wouldn’t improve. They weren’t wrong to worry. Some generic versions of seizure meds, asthma inhalers, or thyroid drugs have different fillers or coatings that affect how fast the drug gets into the bloodstream. For drugs with a narrow therapeutic index - like warfarin or phenytoin - even small changes can matter. A 2017 Danish study followed nine epilepsy patients who switched generics. Three had seizures because the new version absorbed too slowly.What the Law Actually Says (And What It Doesn’t)
The FDA says generics must be bioequivalent. That means they deliver the same active ingredient in the same amount, and the body absorbs it within 80-125% of the brand-name version. That sounds precise. But 20% variation? That’s a lot when you’re giving medicine to a 15-pound toddler or a kidney-weakened 80-year-old. And here’s the kicker: the law doesn’t always protect patients. In 19 states, pharmacists can swap a brand for a generic without telling you. In 7 states and Washington, D.C., they need your consent. In 31 others, they just have to notify you - often with a tiny print slip on the bag. No conversation. No explanation. Just a different pill. The FDA’s own 2019 report admitted that many pediatric drugs go generic without ever being tested in children. If a drug was never studied in kids before it lost its patent, chances are the generic won’t be either. That means a generic version of a reflux medicine for a 3-month-old might be labeled only for adults. The active ingredient is the same - but the formulation? Not tested. Not approved. Not safe.
How to Talk to Parents About Generic Substitutions
Talking to parents isn’t about convincing them generics are “just as good.” It’s about listening to their fears and giving them control. Here’s what works:- Don’t say “It’s the same.” Say: “This medicine has the same active ingredient as the brand, but it’s made by a different company. That’s why it looks different.”
- Ask about past experiences. “Has your child ever had trouble taking a medicine because of how it tasted or felt?”
- Offer alternatives. If the generic liquid is bitter, ask if a chewable tablet or a different brand is available. Some pharmacies stock multiple generic brands - one might be sweeter.
- Use the teach-back method. After explaining, say: “Can you tell me how you’ll give this to your child?” If they say, “I’ll crush it and mix it in applesauce,” stop. That’s not safe for some medications. Correct it now.
- Give a written note. Write the name of the generic, the brand it replaces, and why it’s safe. Parents forget. They’ll show this to their partner, grandma, or babysitter.
How to Talk to Seniors About Generic Substitutions
Seniors need clarity, consistency, and simplicity. Here’s how to help:- Start before the change. Don’t wait until they pick up a pill that looks different. Call or message them ahead of time: “Your blood pressure pill is switching to a new generic next week. We’ll make sure you know what to expect.”
- Use large print and pictures. Give them a card with the old and new pill’s shape, color, and imprint. A photo helps more than words.
- Involve caregivers. If a senior lives alone, talk to their adult child or home care worker. They’re often the ones who notice the pill changed.
- Don’t assume they understand “bioequivalence.” Say: “This pill works just as well as the one you’ve been taking. The only difference is the company that made it. It’s cheaper, but just as safe.”
- Warn them about multiple changes. If their pill changes again next month, say so. “This one might look different again in a few weeks. That’s normal. We’ll let you know each time.”
What to Avoid
Don’t say:- “It’s the same thing.” (It’s not - it’s a different manufacturer.)
- “It’s cheaper, so it’s fine.” (That invites doubt.)
- “Everyone takes generics.” (That dismisses their concern.)
- “The FDA says it’s okay.” (Patients don’t trust agencies. They trust people they know.)
What Works: Real Strategies That Reduce Errors
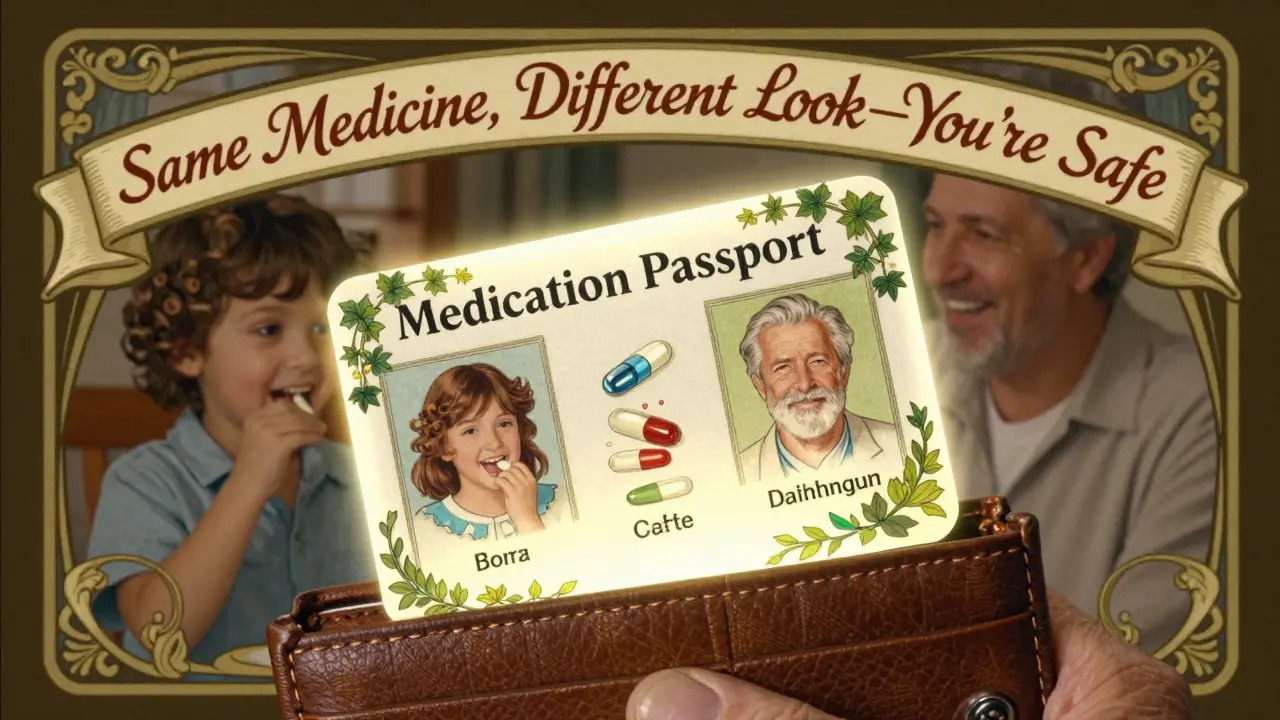
A 2021 NIH study found that using the teach-back method cut medication errors by 29%. That means asking patients to explain back what they heard - in their own words. If a parent says, “So I give this twice a day, and if he spits it out, I don’t give more,” you know they got it. If they say, “I give it when he cries,” you have a problem. Another study in the Journal of the American Pharmacists Association showed that seniors who received a visual pill guide and a phone call before substitution had 32% better adherence. They didn’t stop taking their meds because they didn’t panic. The American Geriatrics Society now recommends a “medication passport” - a small card that lists every drug, its purpose, and its appearance. Seniors keep it in their wallet. When a pill changes, they show it to the pharmacist and say, “Is this the same one?”What’s Changing in 2026
The FDA launched its Generic Drug Communications Initiative in 2023, requiring manufacturers to include clear language about formulation differences in patient materials. In 2024, 28 states started considering laws to block automatic generic swaps for epilepsy, thyroid, and blood thinner drugs in kids and seniors. Some pharmacies now offer digital tools: apps that let you scan your pill and see what it’s supposed to look like. One University of Florida study found 67% of seniors felt more confident using these tools. The bottom line? Generics save the U.S. healthcare system $373 billion a year. But for kids and seniors, the cost of a bad substitution - hospital visits, missed school, falls, seizures - can be far higher. The goal isn’t to stop substitutions. It’s to make them safe. And that starts with how you talk about them.Are generic drugs really as effective as brand-name drugs?
Yes - for most people, generic drugs are just as effective. The FDA requires them to contain the same active ingredient, in the same strength, and deliver it the same way as the brand-name version. But for children and seniors, differences in fillers, coatings, or taste can affect whether the medicine is taken as directed. That’s not about effectiveness - it’s about adherence. If a child refuses to swallow a bitter generic liquid, the drug doesn’t work, no matter how good the science is.
Why do generic pills look different from brand-name ones?
By law, generic manufacturers can’t copy the exact look of a brand-name pill - that’s trademark protection. So they change the color, shape, or imprint. But the active ingredient must be identical. The difference in appearance doesn’t mean the medicine is weaker. It just means it’s made by a different company. Some generics even use different inactive ingredients, which can affect taste or how fast the pill dissolves.
Can I ask for the brand-name drug instead of the generic?
Yes. You can always ask your doctor to write “Dispense as Written” or “Do Not Substitute” on the prescription. This stops the pharmacist from switching to a generic without your permission. But it may mean paying more out of pocket. Some insurance plans won’t cover the brand unless the generic fails or causes a problem. It’s a trade-off between cost and consistency - especially important for kids and seniors.
What should I do if my child or elderly parent refuses to take the generic?
Don’t force it. First, check if the pharmacy has another generic version - sometimes one tastes better or comes in a different form. If not, contact the prescribing doctor. They may be able to prescribe a different medication, adjust the dose, or switch back to the brand if it’s medically necessary. For seniors, a pill organizer with photos of each medication can help reduce confusion. For children, mixing the medicine with a small amount of applesauce or juice (if allowed) can help mask taste.
Is it safe to switch between different generic versions of the same drug?
It’s usually safe, but not always. For drugs with a narrow therapeutic index - like seizure meds, blood thinners, or thyroid pills - even small changes in how the drug is absorbed can cause problems. If you or your loved one is on one of these drugs, ask your doctor if automatic substitution should be avoided. Some states now restrict this for seniors and children. If the pill changes shape or color often, keep a photo log. That way, you can tell your pharmacist or doctor if something feels off.
Next Steps for Families and Caregivers
If you’re managing medications for a child or an older adult:- Ask your pharmacist: “Is this a generic? What brand does it replace?”
- Keep a list of all medications - including what they look like - and update it every time a pill changes.
- Use a pill organizer with clear labels and photos.
- Call your doctor if your child stops taking the medicine or your senior parent reports new side effects after a switch.
- Request a “medication passport” from your pharmacy - a simple card that lists each drug and its appearance.
