Theophylline Levels: Why NTI Monitoring Is Critical for Safe and Effective Treatment
Jan, 26 2026
Theophylline is one of those medications that still saves lives-when it’s used right. Used for decades to treat asthma and COPD, it’s cheap, effective, and surprisingly powerful. But here’s the catch: the difference between helping you breathe and sending you to the ER is razor-thin. That’s why monitoring theophylline levels isn’t optional. It’s non-negotiable.
What Makes Theophylline So Dangerous?
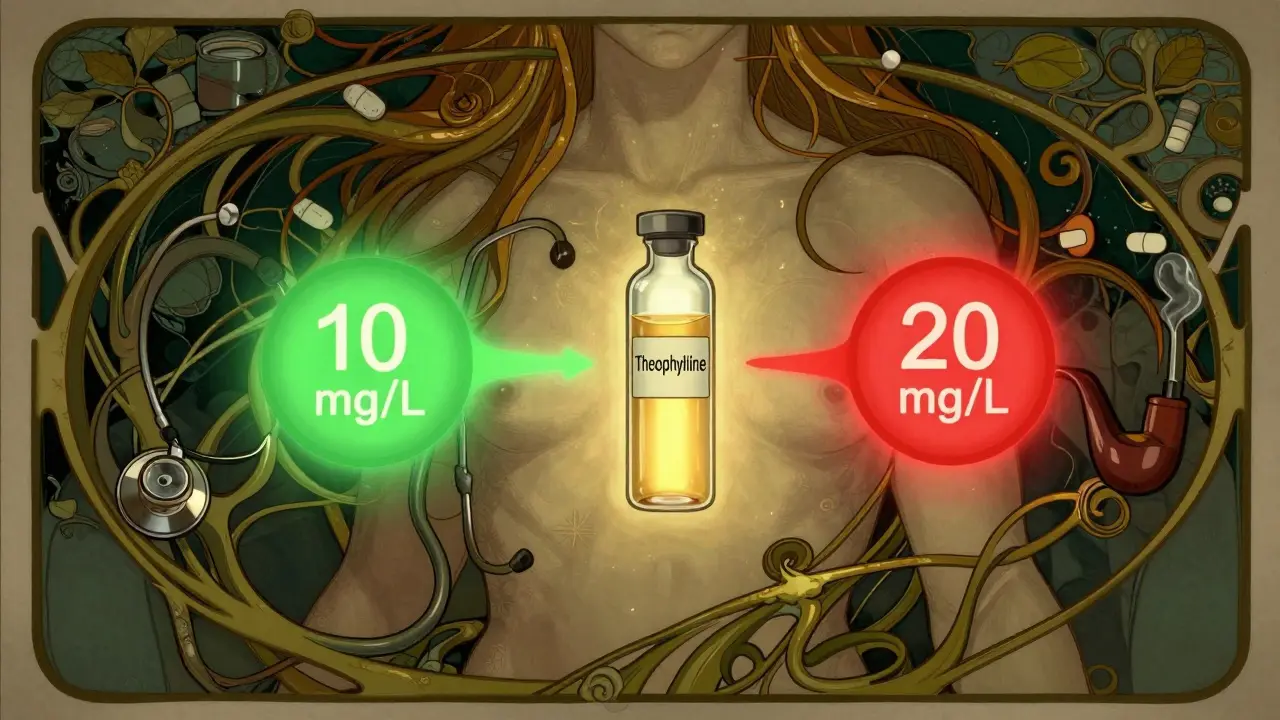
Theophylline works by relaxing the airways and reducing lung inflammation. But its therapeutic window-the range where it works without harming you-is only 10 to 20 mg/L. Go below 10, and it barely helps. Go above 20, and you risk seizures, irregular heartbeat, vomiting, or even death. At levels over 25 mg/L, the chance of serious toxicity jumps sharply.
That’s what makes it an NTI drug-Narrow Therapeutic Index. A tiny change in dose, or a small interaction with another medication, can push you out of safety and into danger. Unlike most drugs, where you can adjust based on how you feel, theophylline doesn’t care how you feel. It only cares about the number in your blood.
Why Your Body Processes Theophylline Unpredictably
Here’s the real problem: your body doesn’t handle theophylline the same way as someone else’s. Even if you and your neighbor take the exact same dose, your blood levels could be completely different.
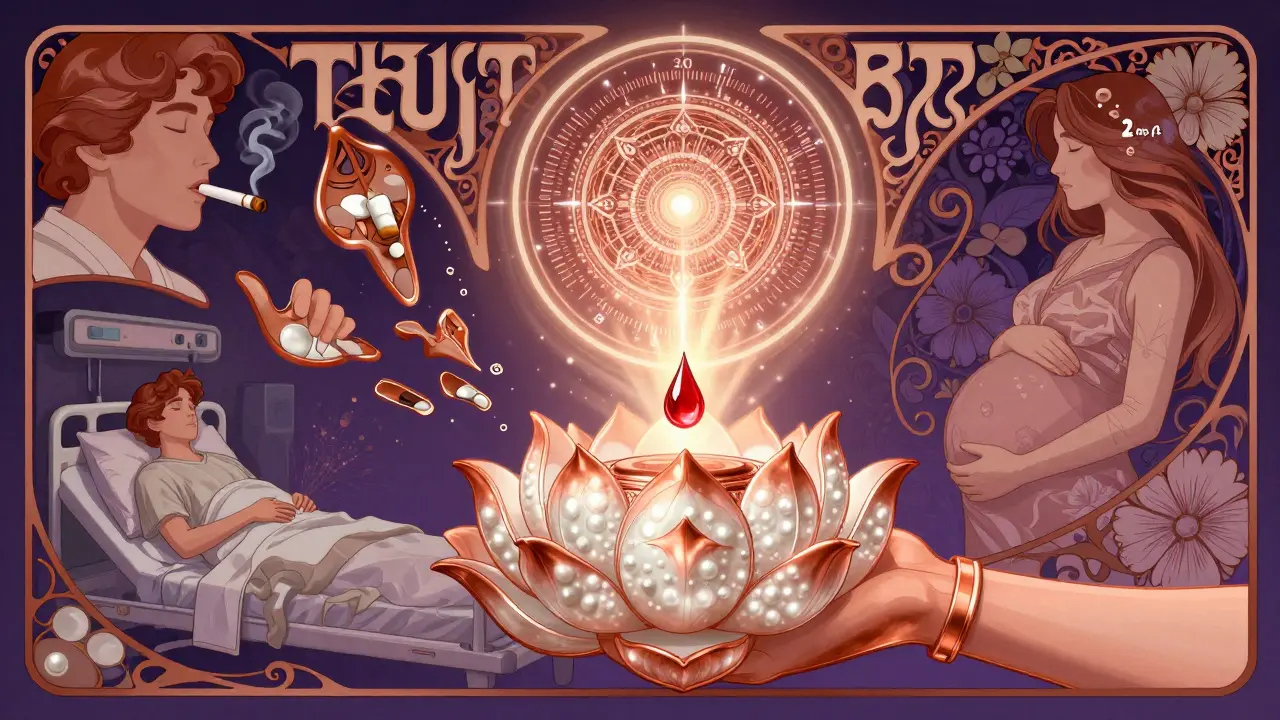
Smokers clear the drug 50-70% faster. That means they often need higher doses just to stay in range. But if they quit smoking, their levels can spike dangerously within days-without any change in pill count.
Older adults? Their livers slow down. By age 60, clearance drops significantly. Patients with heart failure or liver disease? Their bodies can’t process it at all. One study found hepatic impairment cuts clearance by 50% or more.
Pregnancy? Levels drop 30-50% in the third trimester. Stop the drug? No. Adjust the dose? Absolutely. But without testing, you won’t know by how much.
And then there are the drug interactions. Take a common antibiotic like erythromycin or clarithromycin? Theophylline levels can jump 50-100%. That’s not a side effect-it’s a medical emergency waiting to happen. Even cimetidine, a common heartburn pill, can do the same. On the flip side, drugs like carbamazepine or rifampicin can slash levels by 30-60%, making treatment useless.
When and How Often Should You Get Tested?
Testing isn’t a one-time thing. It’s ongoing. Here’s the real-world schedule:
- Start a new dose? Test after 5 days. For modified-release forms, test after 3 days.
- Change your dose? Test again 3-5 days later.
- Stable on treatment? Test every 6-12 months.
- Over 60? Test every 3-6 months.
- Heart failure or liver disease? Test every 1-3 months.
- Pregnant? Monthly during second and third trimesters.
And never skip testing if you start or stop any new medication-even over-the-counter ones. Or if you get sick, stop smoking, or drink more alcohol than usual. These changes can wreck your levels without warning.
Timing matters too. For immediate-release tablets, blood should be drawn right before your next dose-this is the trough level, the lowest point. For extended-release versions, test 4-6 hours after taking it. Get it wrong, and you’ll see a false reading that leads to the wrong decision.

What Else Should Doctors Watch For?
Blood levels alone aren’t enough. You need to look at the whole picture.
- Heart rate above 100 bpm? Could be early toxicity.
- Tremors, insomnia, or nausea? Classic signs.
- Low potassium? Common when you’re also on albuterol or steroids. Low potassium worsens heart risks.
- Abnormal blood gases? Could mean worsening lung function masked by the drug.
- Full blood count? Rare, but theophylline can suppress bone marrow over time.
And if you’re getting theophylline through an IV? Watch the IV site. Mixing it with dextrose solutions can cause clumping or hemolysis-serious complications that can damage veins and trigger reactions.
Real Cases: What Happens When Monitoring Fails
In 2023, a 68-year-old man with COPD started ciprofloxacin for a chest infection. His theophylline level, which had been stable at 14 mg/L, jumped to 28 mg/L in 72 hours. He developed ventricular tachycardia. He survived-but barely. He didn’t know the antibiotic could interact. His doctor didn’t check his levels.
On the flip side, a community hospital in Ohio implemented a strict monitoring protocol in 2022. Within 18 months, the number of theophylline-related ER visits dropped by 78%. Asthma control scores improved by 35%. Patients felt better. Fewer got sick. All because someone finally made testing routine.
According to the NHS, 15% of adverse events happen because doctors didn’t adjust for liver problems. 22% happen because of unmonitored antibiotic interactions. These aren’t rare mistakes. They’re systemic failures.
Why Do We Still Use Theophylline?
It’s not the first choice anymore. New inhalers, biologics, and targeted therapies are safer and easier. But here’s the truth: they’re expensive. Biologics can cost $200-$400 a month. Theophylline? $15-$30. In places without good insurance, or for patients who’ve tried everything else, it’s still a lifeline.
And it’s not just about cost. In severe asthma and COPD, theophylline has unique anti-inflammatory effects-like restoring HDAC2, a protein that helps calm lung inflammation. No other oral drug does this as effectively. That’s why experts still recommend it as a last-line option.
The Future: Will Monitoring Get Easier?
There’s hope. Three companies are testing handheld devices that can measure theophylline levels from a drop of blood in under five minutes. Think of it like a glucose meter-but for theophylline. Phase 2 trials are underway, and if they work, this could change everything.
But right now? That tech isn’t here. And until it is, the only reliable way to know your level is a blood test. The American College of Chest Physicians says it plainly: until point-of-care tests are proven and widely available, serum monitoring remains the standard of care.
The Bottom Line
Theophylline isn’t a drug you take and forget. It’s a tool that needs constant tuning. You wouldn’t drive a race car without checking the oil pressure every few laps. Theophylline is the same. One wrong turn, one missed test, one new pill-and things can go south fast.
If you’re on theophylline, don’t wait for symptoms. Get your levels checked. Tell your doctor every medication you take-even vitamins or herbal supplements. Quit smoking? Let them know. Get pregnant? Tell them. Your life depends on it.
It’s not about being paranoid. It’s about being smart. Because with theophylline, the line between healing and harm is thinner than most people realize.
How often should theophylline levels be checked?
Initial testing should occur 5 days after starting treatment or 3 days after a dose change. For stable patients, check every 6-12 months. Older adults (over 60), those with heart or liver disease, and pregnant individuals need more frequent testing-every 1 to 6 months. Always test after starting or stopping any new medication, changing smoking habits, or experiencing symptoms like nausea, tremors, or palpitations.
What is the safe range for theophylline levels?
The standard therapeutic range is 10-20 mg/L (or μg/mL). Some patients may respond well at lower levels (5-15 mg/L), especially if they’re older or have other health issues. Levels above 20 mg/L increase toxicity risk significantly, and levels over 25 mg/L are considered dangerous, with a high chance of seizures or life-threatening heart rhythms.
Can I stop taking theophylline if I feel fine?
Never stop or adjust your dose without talking to your doctor-even if you feel fine. Theophylline works silently in your body. You might feel okay while your levels are dangerously high or too low. Stopping suddenly can cause rebound breathing problems. Always follow your prescribed schedule and get regular blood tests to confirm your levels are safe.
What medications interact with theophylline?
Many common drugs affect theophylline. Antibiotics like erythromycin and clarithromycin can raise levels by 50-100%. Cimetidine (for heartburn), allopurinol, and fluvoxamine also increase risk. On the other hand, carbamazepine, rifampicin, and St. John’s Wort can lower levels by 30-60%. Even smoking and alcohol change how your body processes it. Always tell your doctor every medication, supplement, or lifestyle change.
Is theophylline still used today?
Yes, but only as a third-line option for severe asthma or COPD that doesn’t respond to inhalers or biologics. It’s still used because it’s affordable ($15-$30/month) and has unique anti-inflammatory effects. About 1.2 million people in the U.S. and 850,000 in Europe still take it. However, its use is declining as safer alternatives become more accessible.
What are the signs of theophylline toxicity?
Early signs include nausea, vomiting, headache, insomnia, and tremors. More serious signs are rapid or irregular heartbeat (over 100 bpm), confusion, seizures, and chest pain. If you experience any of these, stop the medication and seek medical help immediately. Toxicity can progress rapidly and become fatal without treatment.
Why can’t I just rely on how I feel?
Because theophylline doesn’t work like most drugs. You can feel fine while your blood level is dangerously high-or you can feel awful while your level is perfectly safe. Symptoms don’t match up with blood concentrations reliably. Only a blood test can tell you if you’re in the safe range. Relying on how you feel is how people end up in the ER.
Are there alternatives to theophylline?
Yes. Inhaled corticosteroids, long-acting beta-agonists, and biologic therapies like omalizumab or mepolizumab are now preferred because they’re safer and don’t require blood monitoring. But they’re expensive. Theophylline remains a vital option for patients who can’t afford these drugs or whose condition hasn’t responded to other treatments.
