Hypertension in Pregnancy: Risks, Management, and What You Need to Know
When hypertension in pregnancy, a condition where blood pressure rises during pregnancy, often without clear symptoms until it becomes dangerous. Also known as gestational hypertension, it affects up to 1 in 10 pregnant women and can lead to serious problems for both mother and baby if ignored. It’s not just high blood pressure—it’s a signal that something deeper may be going on in your body during one of the most critical times in your life.
This isn’t the same as chronic high blood pressure you had before pregnancy. preeclampsia, a dangerous pregnancy complication marked by high blood pressure and signs of organ damage, often the liver or kidneys is the most serious form. It usually shows up after 20 weeks and can cause seizures, stroke, or even death if untreated. Then there’s gestational hypertension, high blood pressure that develops after 20 weeks without protein in the urine or organ damage. It doesn’t always turn into preeclampsia, but it still needs watching. Both types can restrict blood flow to the placenta, slowing your baby’s growth or triggering early labor.
What makes this tricky is that many women feel fine. No headaches. No swelling. No warning. That’s why regular checkups aren’t optional—they’re life-saving. Your doctor checks your blood pressure at every visit, tests your urine for protein, and watches for sudden weight gain. If your numbers creep up, they might start you on safe medications like methyldopa or labetalol. Lifestyle changes matter too: cutting back on salt, staying active, avoiding stress, and sleeping on your left side can help lower pressure naturally.
Some women worry about taking meds during pregnancy. But uncontrolled hypertension is far riskier than most approved treatments. The goal isn’t to get your numbers perfect—it’s to keep you and your baby safe until delivery. In severe cases, early delivery might be the best option, even if your baby isn’t full-term. It’s not a failure. It’s a smart move.
You’re not alone in this. Many women go through it. Some have no symptoms at all. Others feel exhausted, get headaches, or notice their face or hands swelling. If you notice sudden swelling, blurry vision, pain under your ribs, or a bad headache after 20 weeks, don’t wait. Call your provider. That’s not anxiety—that’s your body screaming for help.
The posts below cover real cases, medication options, warning signs you can’t ignore, and how to manage this condition without panic. You’ll find practical advice on what to eat, what to avoid, how to track your numbers at home, and when to push for more testing. No fluff. No fearmongering. Just clear, actionable info from people who’ve seen this firsthand.
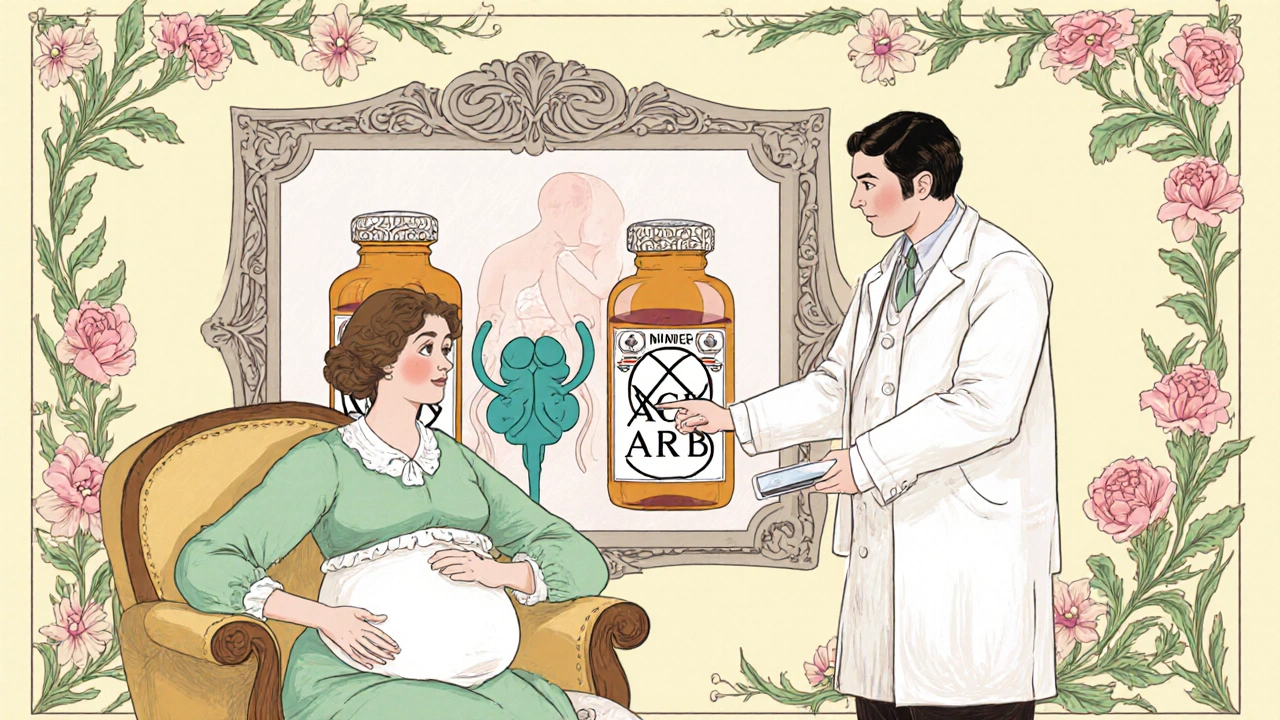
Pregnancy Risks of ACE Inhibitors & ARBs and Safer Alternatives
Caspian Mortensen Oct, 26 2025 8Learn why ACE inhibitors and ARBs are dangerous in pregnancy, see the real fetal risks, and discover safe antihypertensive alternatives with step‑by‑step switching guidance.
More Detail