Therapeutic Equivalence: What It Means and Why It Matters for Your Medications
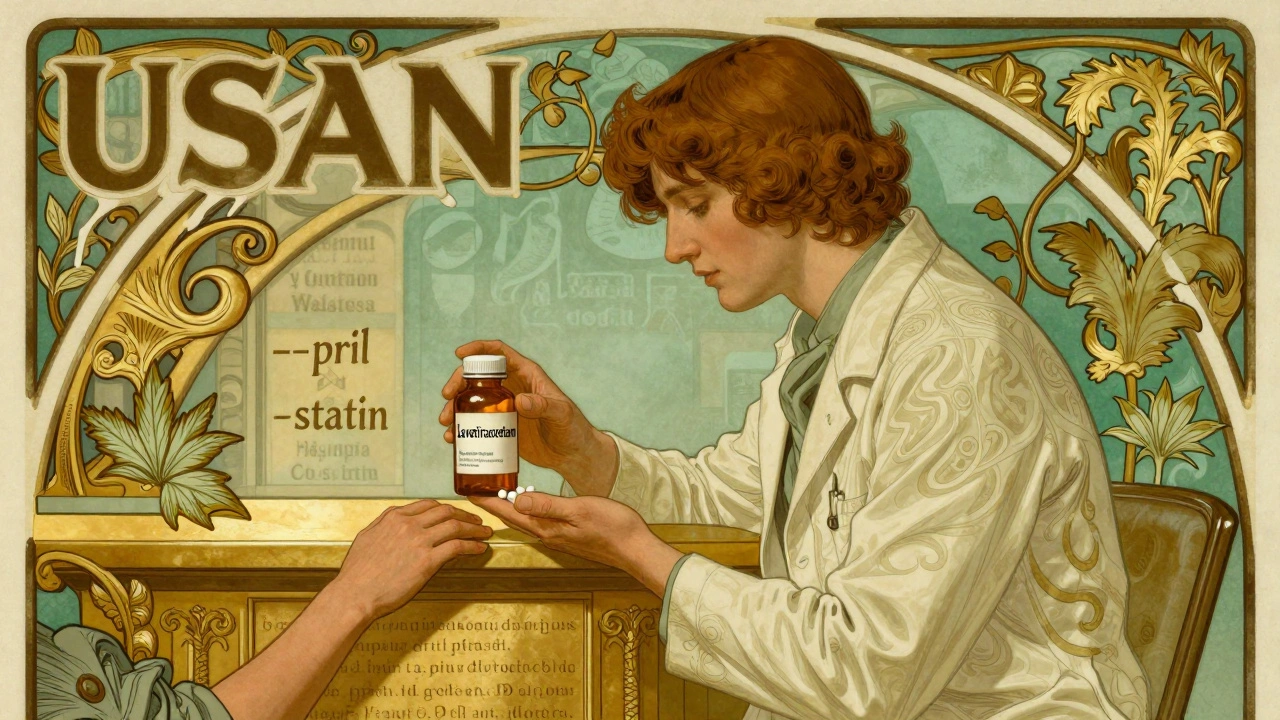
When you hear therapeutic equivalence, the official term used by the FDA to say two drugs produce the same clinical effect and safety profile in patients. Also known as bioequivalence, it's the reason your pharmacist can legally swap a brand-name pill for a cheaper generic without asking your doctor. This isn't just paperwork—it’s what keeps your prescriptions affordable and your treatment on track.
Therapeutic equivalence isn’t about looking the same or costing less. It’s about proving, through strict testing, that the generic version releases the same amount of active ingredient into your bloodstream at the same speed as the brand. The FDA, the U.S. agency that evaluates drug safety and effectiveness does this with real human studies and lab data. If a drug meets the standard, it gets an AB rating in the Orange Book—meaning it’s interchangeable. But not all generics are rated that way. Some have AB1, AB2, or even no rating at all. That’s why you can’t assume every generic is a direct swap—especially with narrow-therapeutic-index drugs like warfarin or thyroid meds.
What makes therapeutic equivalence so powerful is how it connects to real-world savings. When multiple generic manufacturers enter the market, competition drives prices down—sometimes by 80%. That’s why generic drug competition, the process where multiple companies produce the same medication after patent expiry is a major reason Medicare and insurers save billions every year. But it only works if those generics are truly equivalent. If one batch performs differently, it can throw off your treatment, cause side effects, or even lead to hospital visits. That’s why the FDA monitors lot-to-lot consistency, especially with complex drugs like biologics and injectables.
You might wonder: if generics are the same, why do some people say they feel different? Sometimes it’s the filler ingredients—dyes, binders, or coatings—that cause minor reactions. But that’s not therapeutic failure. That’s individual sensitivity. The science still holds: if two drugs are rated AB, they’re clinically interchangeable. Your body doesn’t care if it’s made by Pfizer or Teva—it cares about the active ingredient, its dose, and how fast it gets into your system.
Therapeutic equivalence also ties into how you get your meds. Whether you’re using a 90-day fill to save money, switching from brand to generic after a prescription change, or checking your OTC labels for hidden active ingredients, this concept is the silent backbone of safe, affordable care. It’s why pharmacists can confidently substitute, why insurance plans require generics first, and why you can trust that your $4 monthly pill does the same job as the $200 one.
Below, you’ll find real-world examples of how therapeutic equivalence plays out in daily life—from antibiotic timing and drug interactions to how patent challenges and sourcing rules protect your access to safe, effective generics. These aren’t abstract rules. They’re the reason you’re still able to afford your meds without guessing if they’ll work.
Medical Society Guidelines on Generic Drug Use: What Doctors Really Think
Caspian Mortensen Dec, 8 2025 15Medical society guidelines on generic drug use vary by specialty and drug type. While most generics are safe and effective, some drugs - especially those with narrow therapeutic indices - require caution. Learn what doctors, pharmacists, and regulators really think about substitution.
More Detail